Nutrition
- a basic human need
Nutritional status assessment
- anthropometrical examination (weight, height, BMI, waist circumference measurement, measurement of the circumference of the muscles on the non-dominant arm, measurement of skin fold thickness)
- biochemical markers – blood and urine examination
- clinical indicators – body constitution, symptoms of malnutrition, hydration status
- nutritional history – eating habits
Nutritional care
- provided by nutrition team, multidisciplinary team – dietitian, nurse, doctor, hospital attendant, health care assistant, hospital catering provider
- dietitian – performs nutritional diagnostics, solves nutritional problems, consults a doctor, suggests and evaluates nutritional measures
- nurse – recognizes, monitors and solves nutritional problems
- doctor – performs nutritional screening at admission, assesses nutritional status, orders dietary measures and solves nutritional problems
- hospital attendant, health care assistant – assists with food distribution, monitors food consumption
- food service – personalizes the diet according to the patient's needs
Dietary system
Diet
- Part of the treatment regime
- food individualized according to the doctor's orders
- requirements – food has energy and biological value, is harmless in hygienic-epidemiologic sense, and is tasty, diverse, warm, and aesthetically pleasing
Basic Diets
| Diet number | Diet designation | Energy kJ | Indication |
| 0 | full – liquid | 6 000 | short-term administration; after oral cavity surgery; pharyngeal and oesophageal diseases, swallowing disorders; after tonsillectomy, jaw injuries or dental operations |
| 1 | pureed | 9 500 | chest and swallowing disorders (seniors, conditions after radiotherapy and chemotherapy); acute attack of gastric and duodenal ulcer disease; injuries and surgical procedures in oral cavity, throat or oesophagus |
| 2 | soft | 9 500 | gastric and duodenal diseases; after heart attack; skin diseases; allergies |
| 3 | regular | 9 500 | all foods, no restrictions |
| 4 | fat-modified | 9 500 | diseases of the liver, gallbladder and pancreas |
| 5 | low-residue | 9 500 | inflammatory bowel disease; intestinal surgery; diarrhoea after radiotherapy and chemotherapy |
| 6 | low-protein | 9 500 | kidney disease |
| 8 | slimming | 5 300 | overweight, obesity |
| 9 | diabetic (consistent carbohydrate diet) | individual | diabetes mellitus |
| 10 | low-sodium | 9 500 | hypertension; swelling; heart and blood vessel diseases |
| 11 | high-nutritional | 12 000 | malnutrition; cachexia; re-alimentation, convalescence; cancer; irradiation, polytrauma |
| 12 | toddler food (age 1–3 years) | 7 000 | normal diet, composition and consistency adjusted for the toddlers |
| 13 | children's food (age under 15) | 9 500 | normal diet, modified to children |
| 14 | selective diet | 9 500 | malnutrition; cachexia; mental anorexia, bulimia; selection of meals according to patient's wishes (provided by the nutrition therapist) |
* diet No. 7 (low-cholesterol) – is no longer included in the dietary system as of 2008 (every diet should have low cholesterol content)
Special diets
| Diet number | Diet designation | Indication |
| 0-S | tea | tea in sips |
| 1-S | liquid high-nutritional | chest and swallowing disorders + need of increased energy intake (seniors; conditions after radiotherapy and chemotherapy; injuries and surgical procedures in oral cavity, throat or oesophagus |
| 4-S | strict fat limitations | acute hepatitis; acute gallbladder inflammation; after cholecystitis; after cholecystectomy; after starving in pancreatitis |
| 9-S | diabetic soft | diabetes mellitus with concomitant diseases of the digestive tract |
| W | warfarin | when treated with warfarin, diet with vitamin K excluded (no green leafy vegetables) |
| KVM | vanillylmandelic acid | when measuring vanillylmandelic acid content, fruits, vegetables and fruit juices are excluded |
Standardized dietary procedures
| Diet number | Diet designation | Indications |
| BLP | gluten-free | celiac disease; sprue |
| BL | lactose-free | lactose intolerance |
| P | pancreatic | gradual alimentation after pancreatitis |
| OK | occult bleeding diet | before examination of occult (hidden) bleeding from GIT |
Enteral nutrition
- administration of pharmaceutically prepared nutritional products
- purpose – maintaining good nutritional status, improving nutritional status
- proper functioning of gastrointestinal tract is an essential precondition here
Methods of application
- sipping
- nourishment via the nasogastric feeding tube
- nourishment via naso-enteric feeding tube
- PEG – percutaneous endoscopic gastrostomy
- PEJ – percutaneous endoscopic jejunostomy
- feeding tube introduced surgically – jejunostomy, gastrostomy
Enteral Nutrition Products
- sipping products
- polymeric (high molecular weight) products
- polymeric modified products – modified for specific diseases
- oligomeric (low-molecular) products
Advantages
- stimulation of digestive tract motility and secretion of hormones and enzymes
- avoiding mucosal atrophy, maintaining a natural immunological barrier and bacterial balancea
- lower costs than parenteral nutrition
Sipping
- the simplest form of enteral nutrition
- liquid products (Nutridrink, Diasip, Cubitan, Fresubin, etc.)
- products containing individual (single) nutrients or all components of nutrition
Principles
- explain to the patient the reasons for and the method of administration; patient drinks in small sips during the day – prevention of diarrhoea and nausea
- specially prepared sipping products – for a patient with non-healing wounds, oncological diseases, or dietary restrictions (Diasip for diabetes mellitus patients; Nutridrink Juice Style for fat-free nutrition; Nutridrink Multi Fibre for patients needing fibre, etc.)
- product temperature – according to the patient (colder sipping reduces nausea, promotes appetite)
- oncological patients during chemotherapy – alternate only two flavours to prevent aversion to flavours; useful in cases of nausea due to chemotherapy
Nasogastric tube (NG)
Provides nutrition
- nutritionally and chemically defined products are used
- a thin polyurethane or silicone tube is inserted
- Leave the tube inside for maximum 4–6 weeks; after 14 days a replacement or change of position is recommended to prevent pressure ulcers.
NG tube for gastric decompression
- inserting a thick PVC tube
- suction of stomach contents (monitoring the character and amount of secretions)
- gastric lavage in case of intoxication
- short-term (up to 7 days)
- NG tube positioning – prevention of pressure ulcers
Contraindications of NG tube use
- anatomical obstructions; acid burning of oesophagus; severe mucosal bleeding; risk of perforation of the oesophagus and stomach
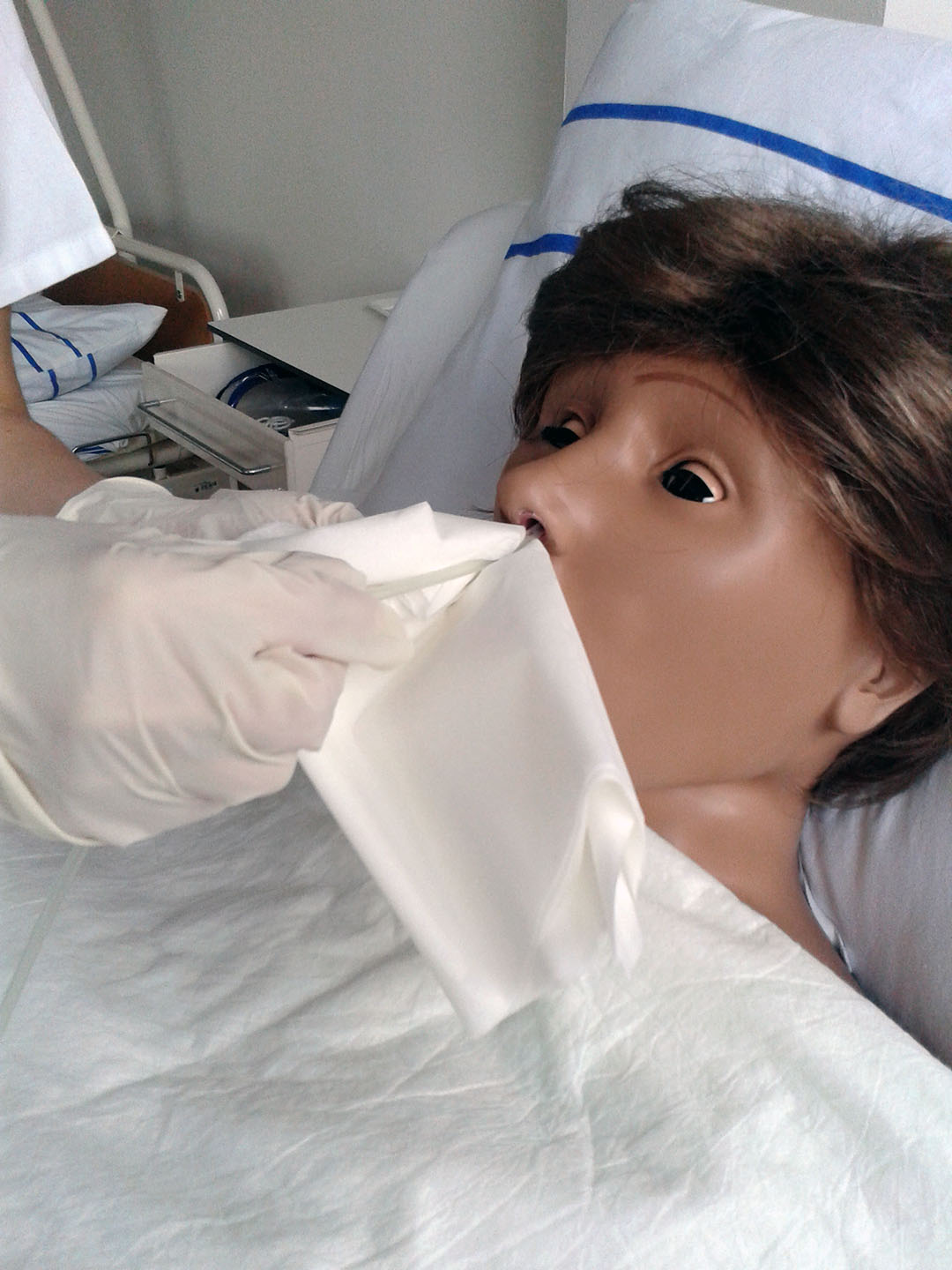
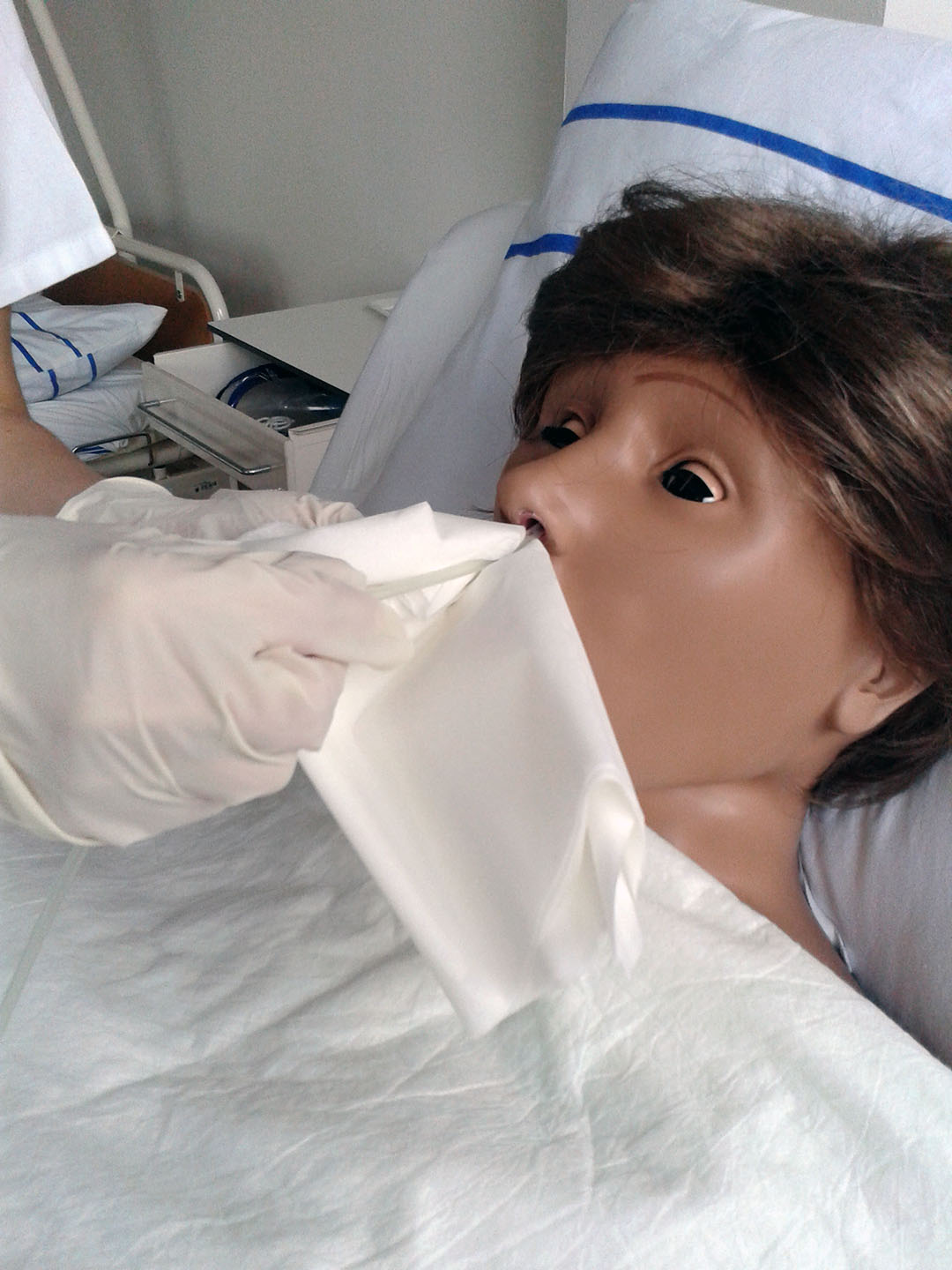
Nasogastric tube insertion
- competence – general nurse without professional supervision, according to the doctor's indication, for conscious patients 10 years and older
1) Preparation of the patient
- semi-Fowler's (low Fowler's) position
- Blow the patient's nose.
- Assess nostril space.
- Remove and store dental prosthesis.
- Instruct the patient to breathe through the nose, swallow, then breathe out.


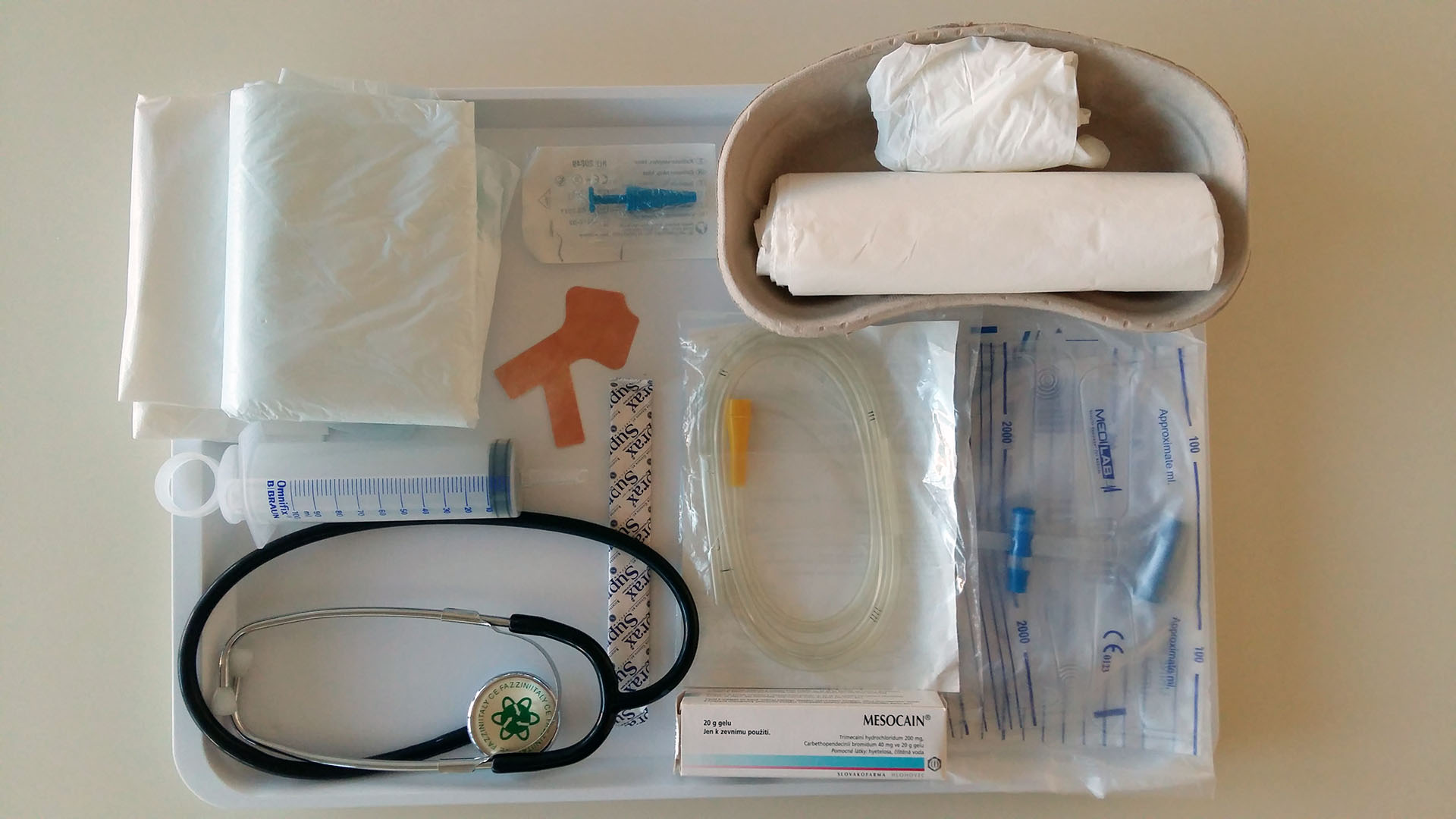
*do not store the equipment in a kidney dish
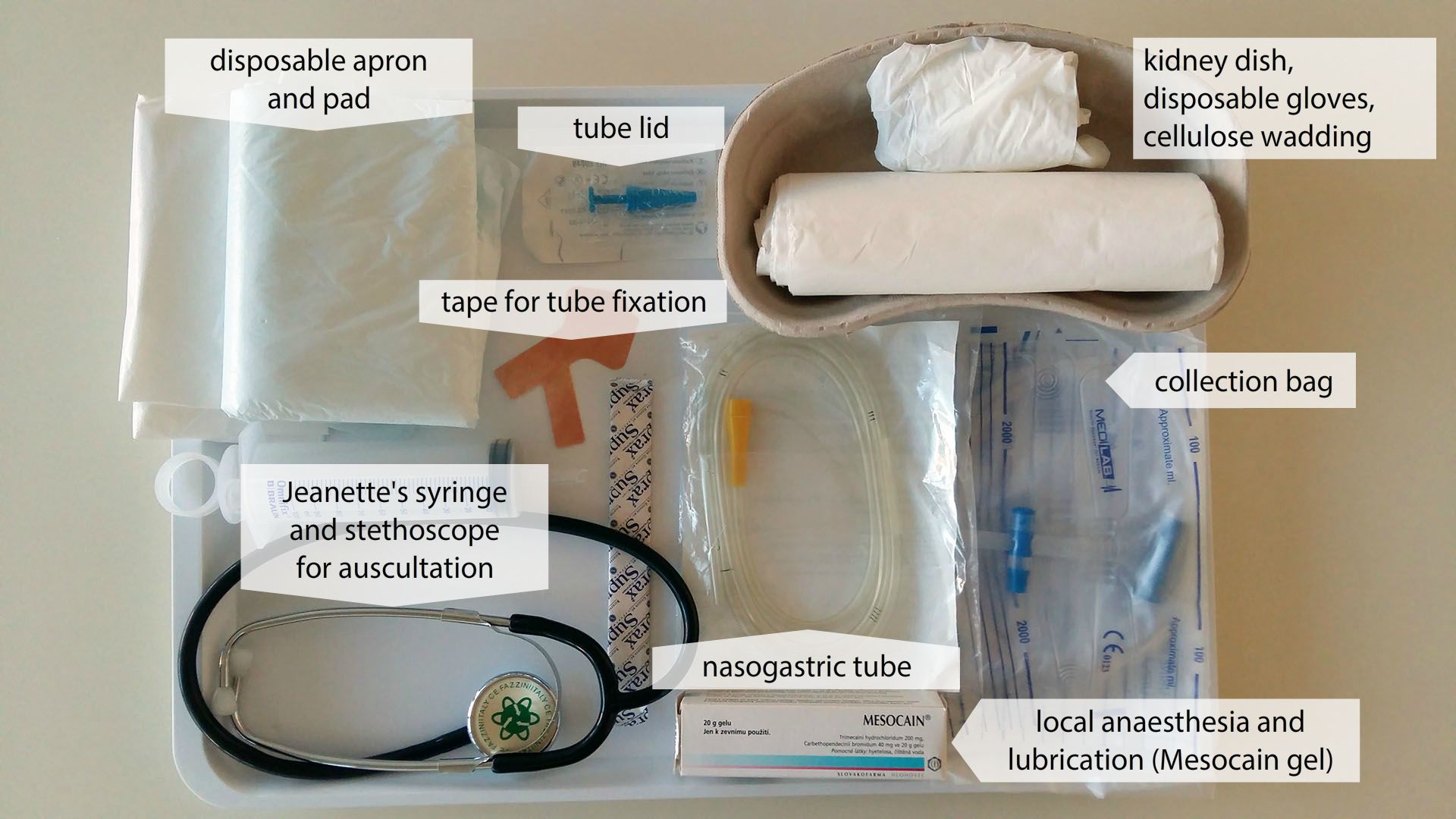
*do not store the equipment in a kidney dish
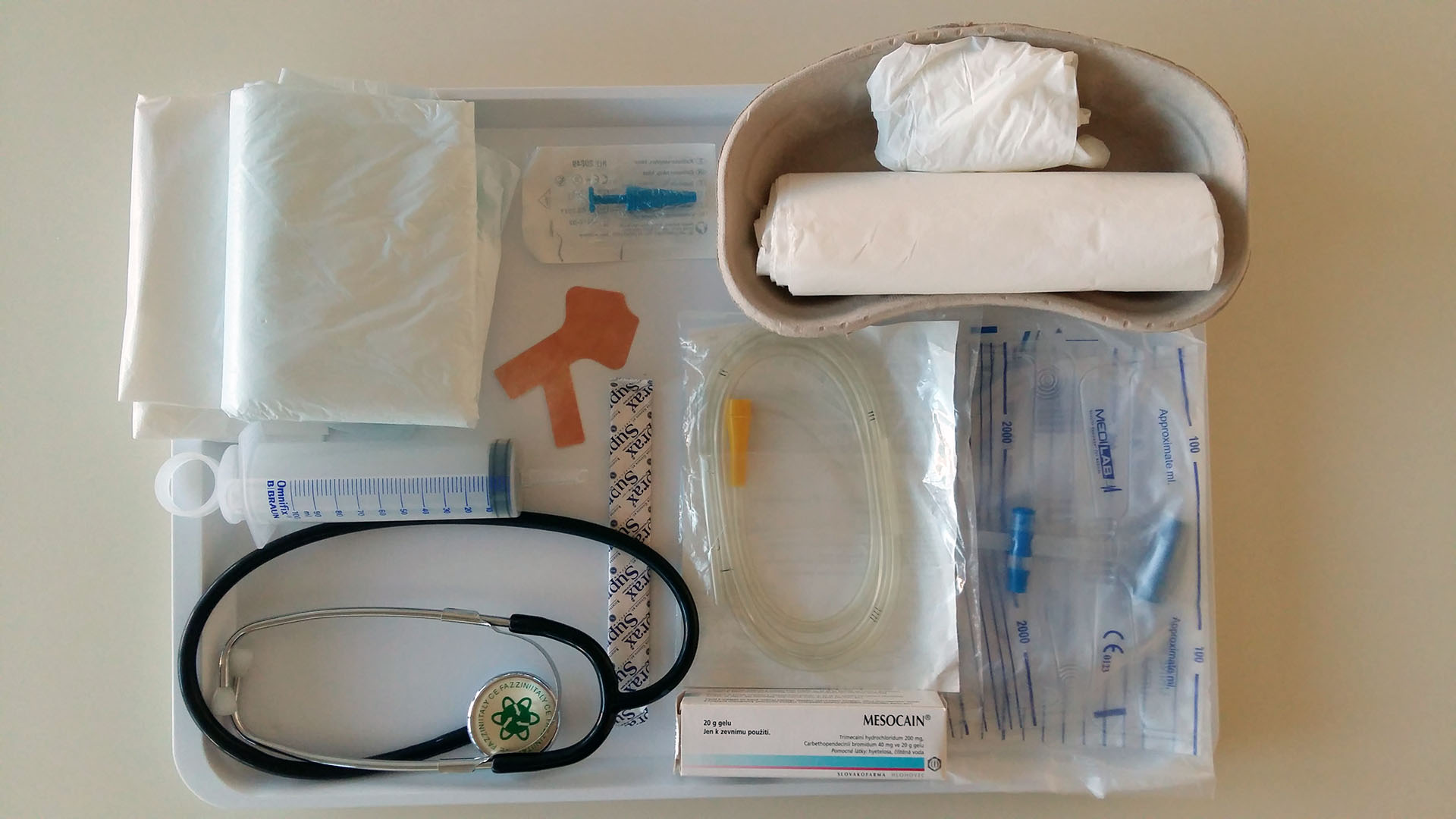
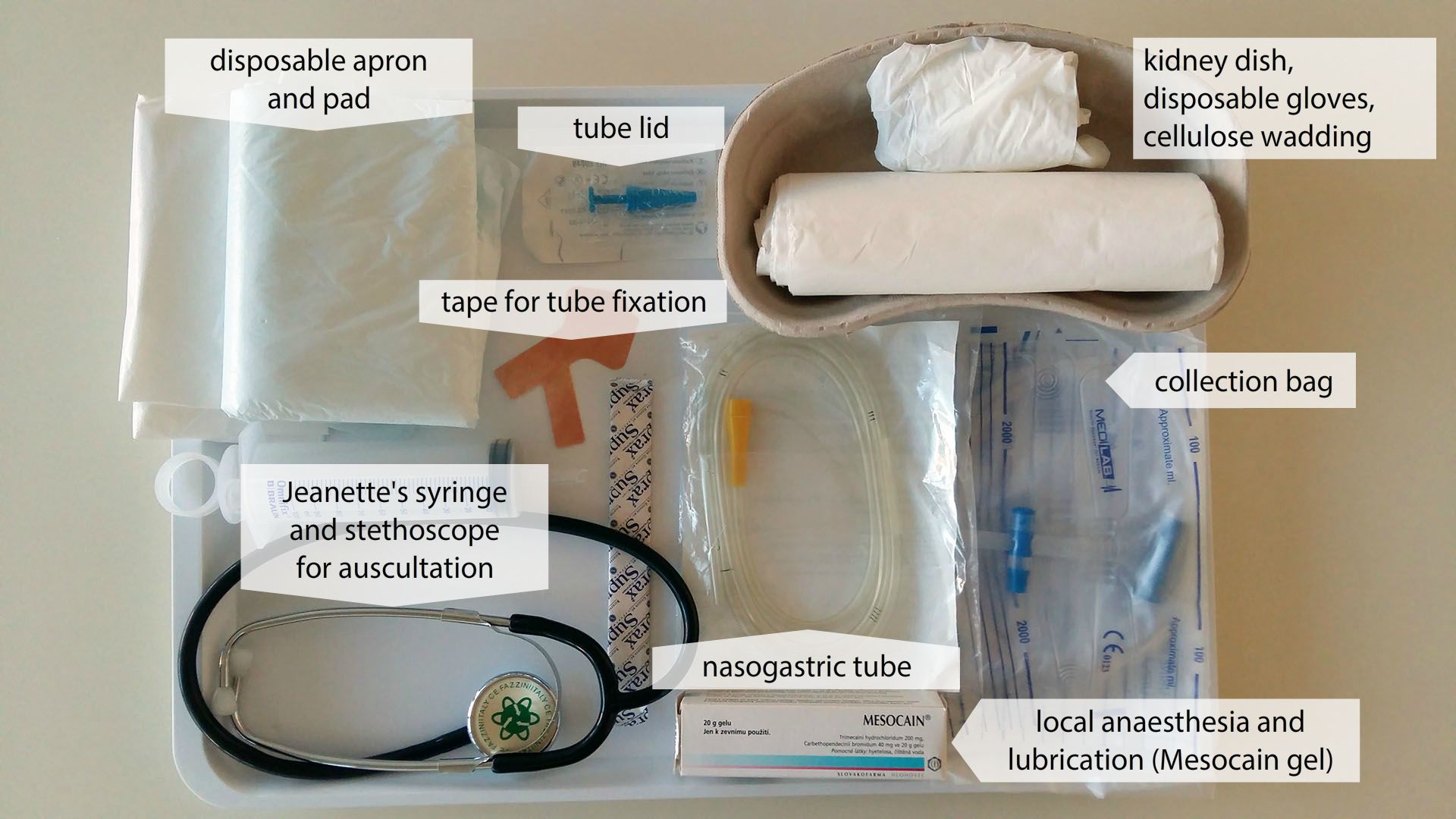
2) Insertion of nasogastric tube
- position the patient – semi-Fowler's position – first have patient raise head, then after tube has passed through nasopharynx, have patient lower head. Patient takes a breath, then swallows (we advance the nasogastric tube during swallowing), then breathes out. Breathing and swallowing cycles to be repeated up to the indicated length on the NG tube). If the patient feels sick during insertion of NG tube, interrupt the procedure, let him/her take breath, make lessening the patient's anxiety a priority
- the correct length – from the xiphoid process of the sternum behind ear and to the tip of the nose, mark on the NG tube
- local anaesthesia – Mesocain gel
- NG tube can be stored in the freezer for approximately 30 minutes before insertion for easier insertion.


3) Verify the correct location
- auscultation – stethoscope on the xiphoid process of the sternum, inject 30 mL of air with Jeanette syringe – audible air bubbling
- Examine the pH of the aspirated gastric content by using pH indicators, physiological range 0–4; when introduced into the respiratory tract, the content has straw colour, pH 6–8.
- X-ray control
4) Details recorded in the documentation
Removal of the nasogastric tube
- on the basis of a doctor's orders
- undesired removal by the patient
- Before removal, clamp the NG tube according to the doctor's orders (e.g. one hour before removal or one day before; observe the patient – flatulence, belching, nausea, etc.).
- Insufflate 30 – 50 mL of air to prevent residue in NG tube.
- Instruct the patient – take a deep breath, hold breath, pull NG tube out.
- Record details in the documentation.
Administering enteral nutrition
Bolus administration
- between 6 am – 10 pm for 2–3 hours, Jeanette syringe, 150–300 mL of prescribed enteral formula
- overnight break
- room-temperature nutrition
- patient in semi-Fowler's position
- aspiration of the stomach content, over 100 mL skip the following dose, return the aspirated content back to the stomach (contains gastric juices)
- adequate speed and pressure of delivery
- Flush the tube with boiled water and close for 30 minutes, the patient should be in semi-Fowler's position after administration.
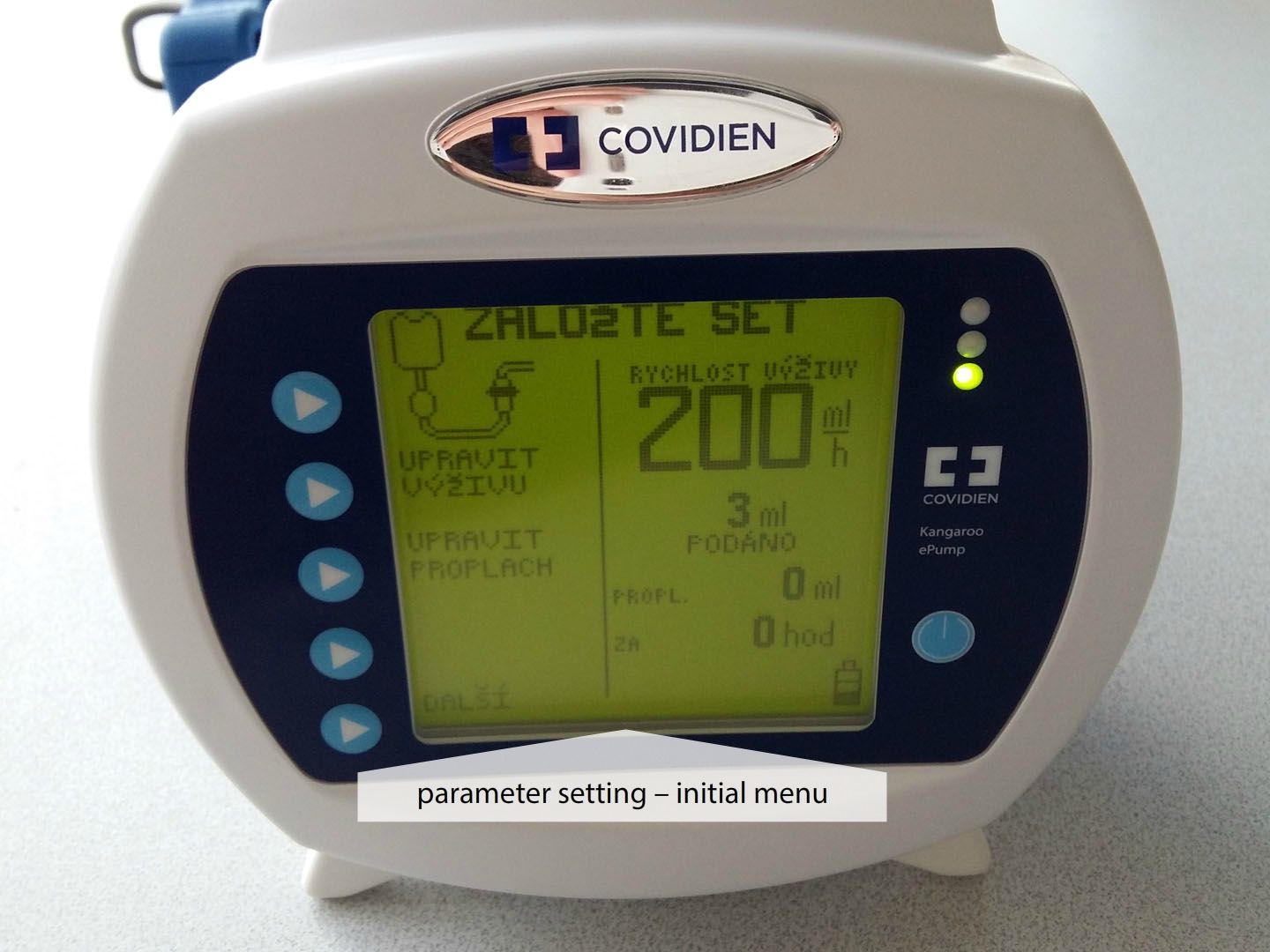
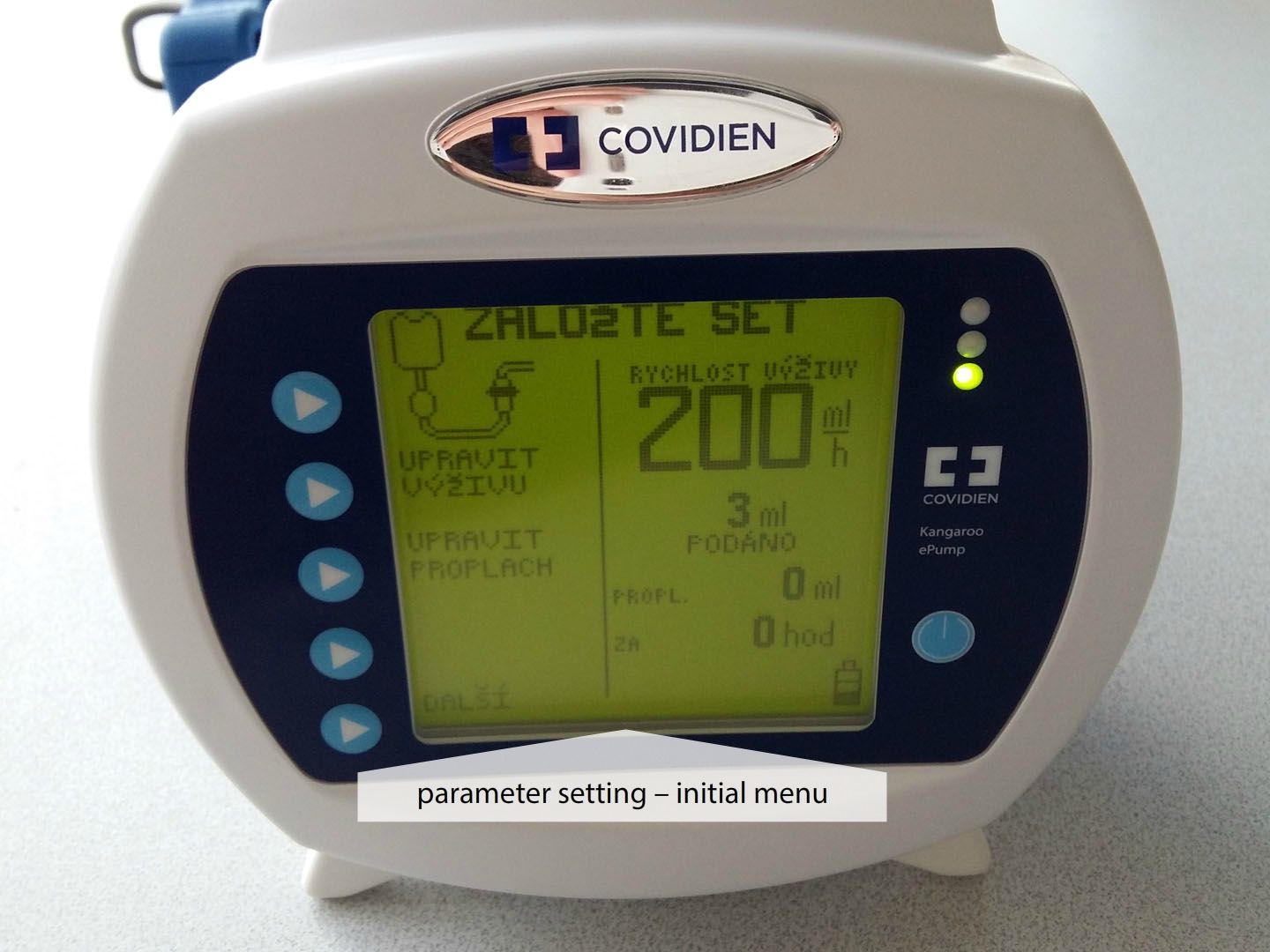
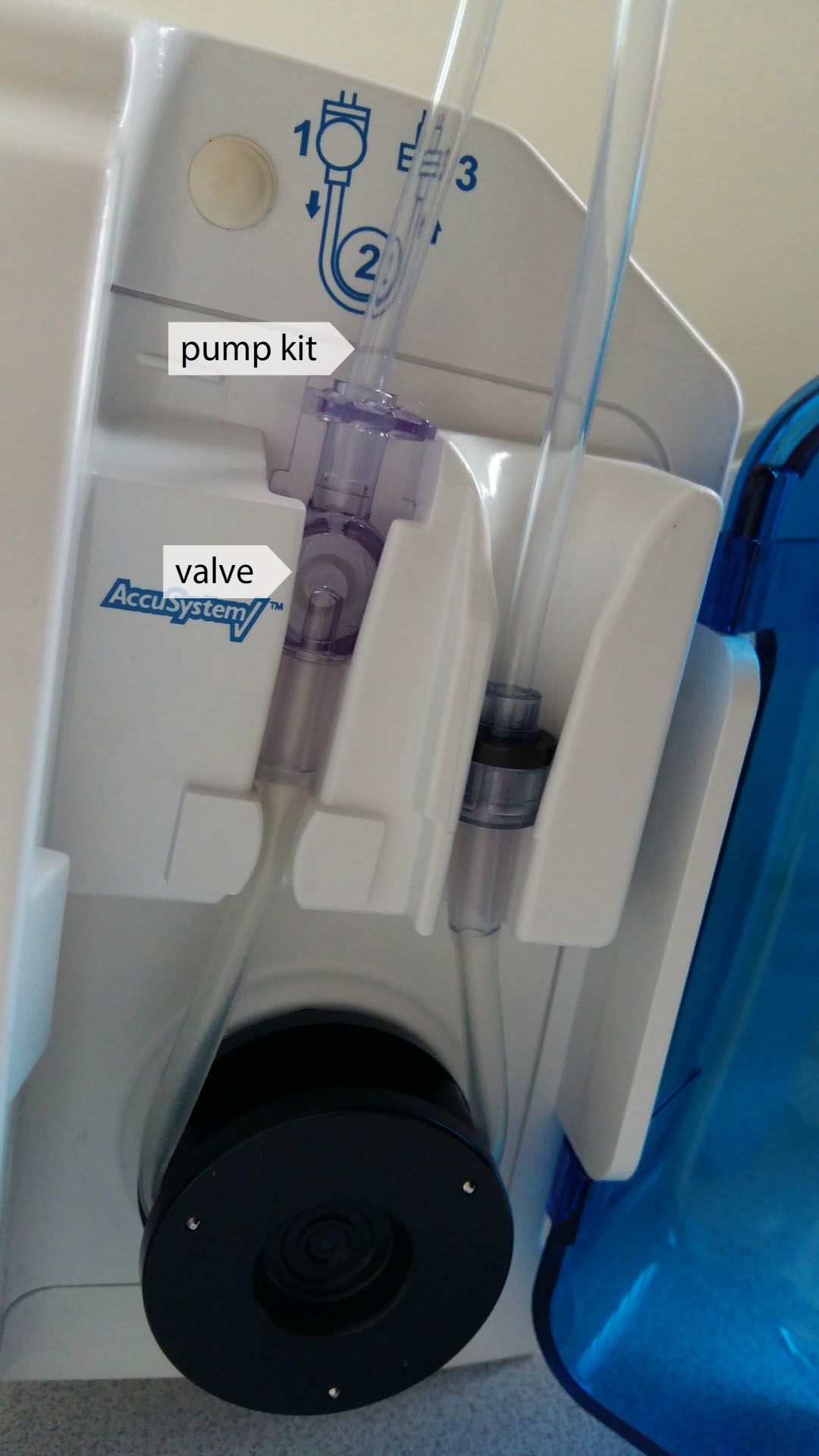
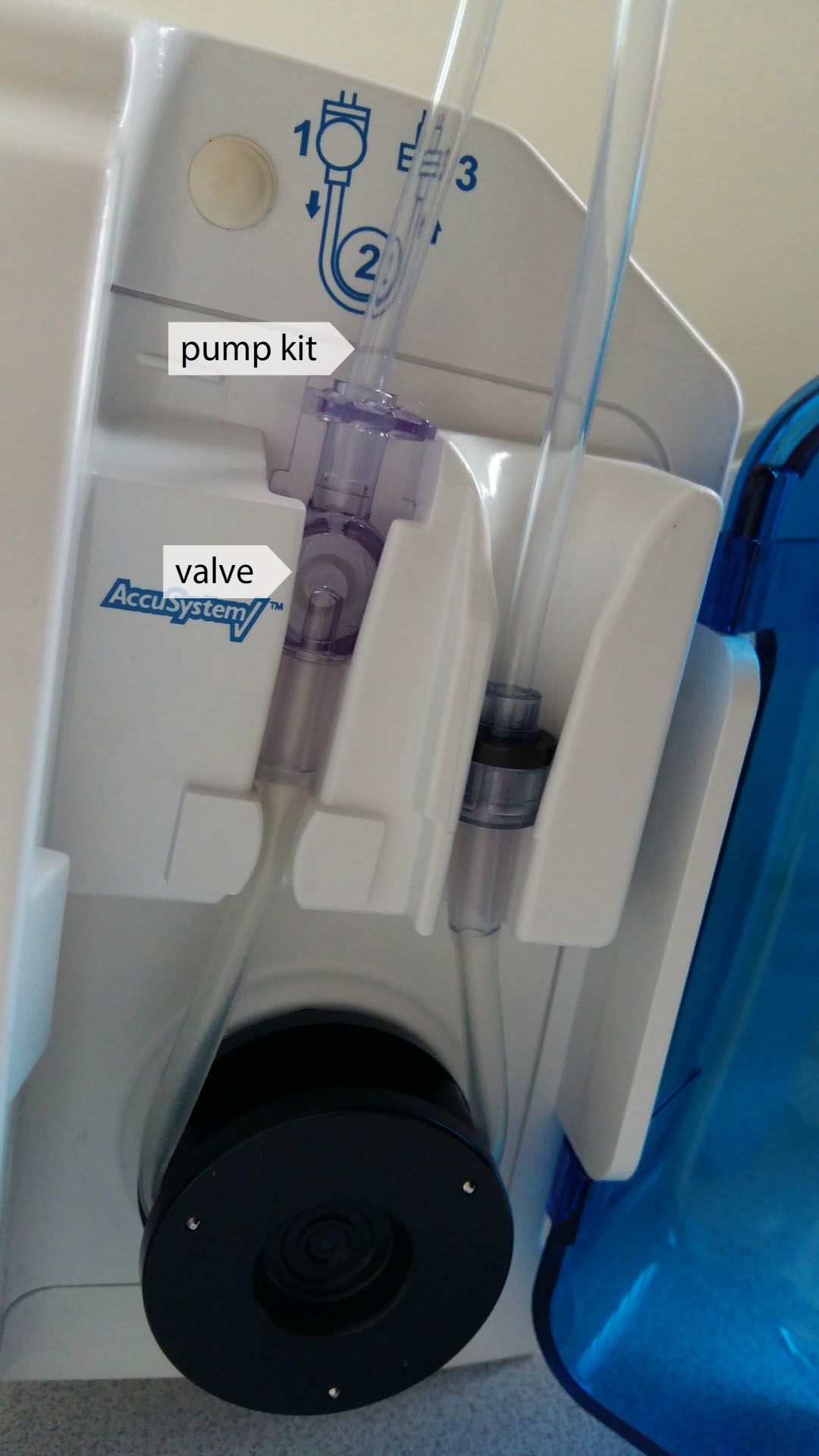
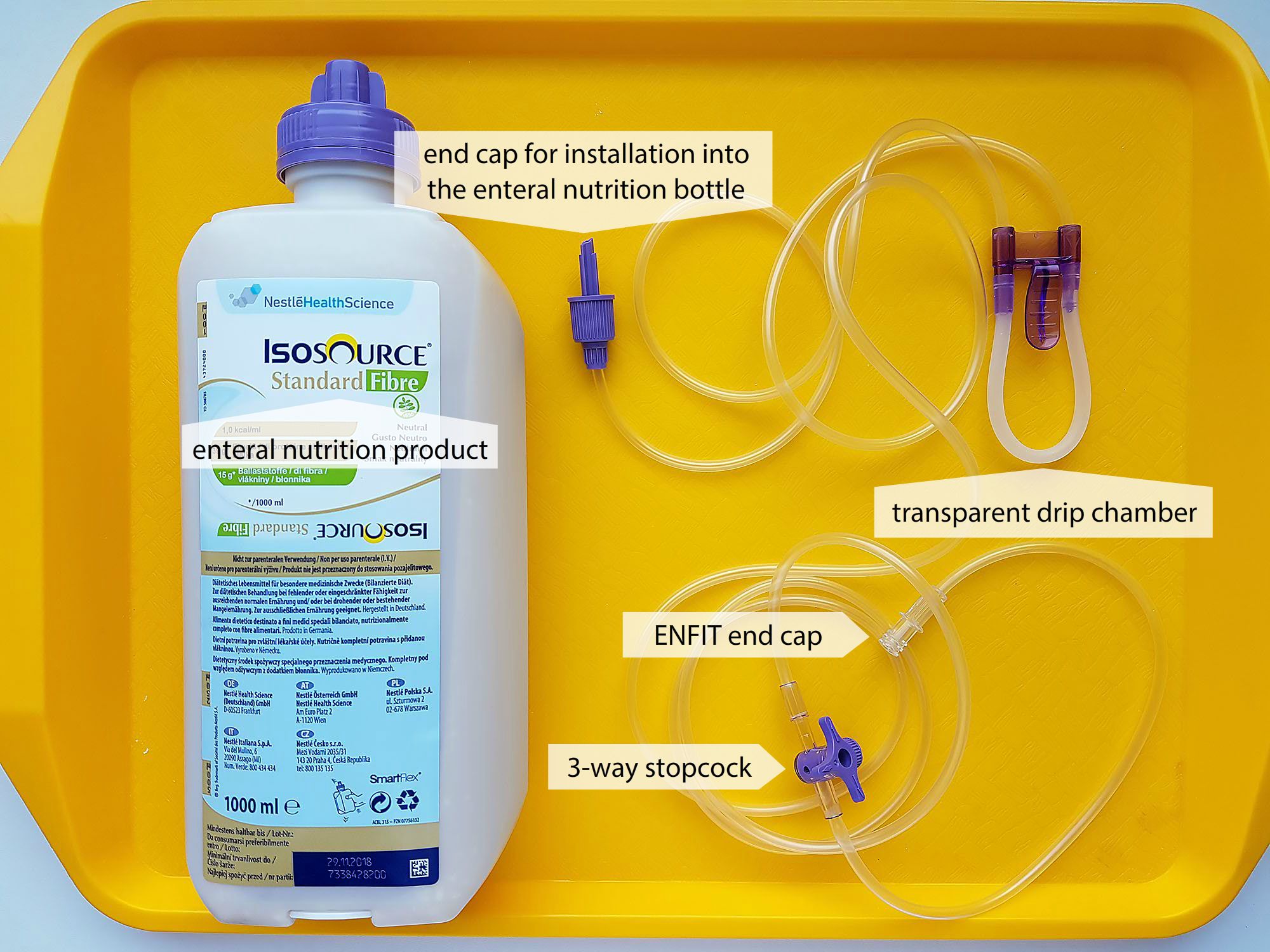
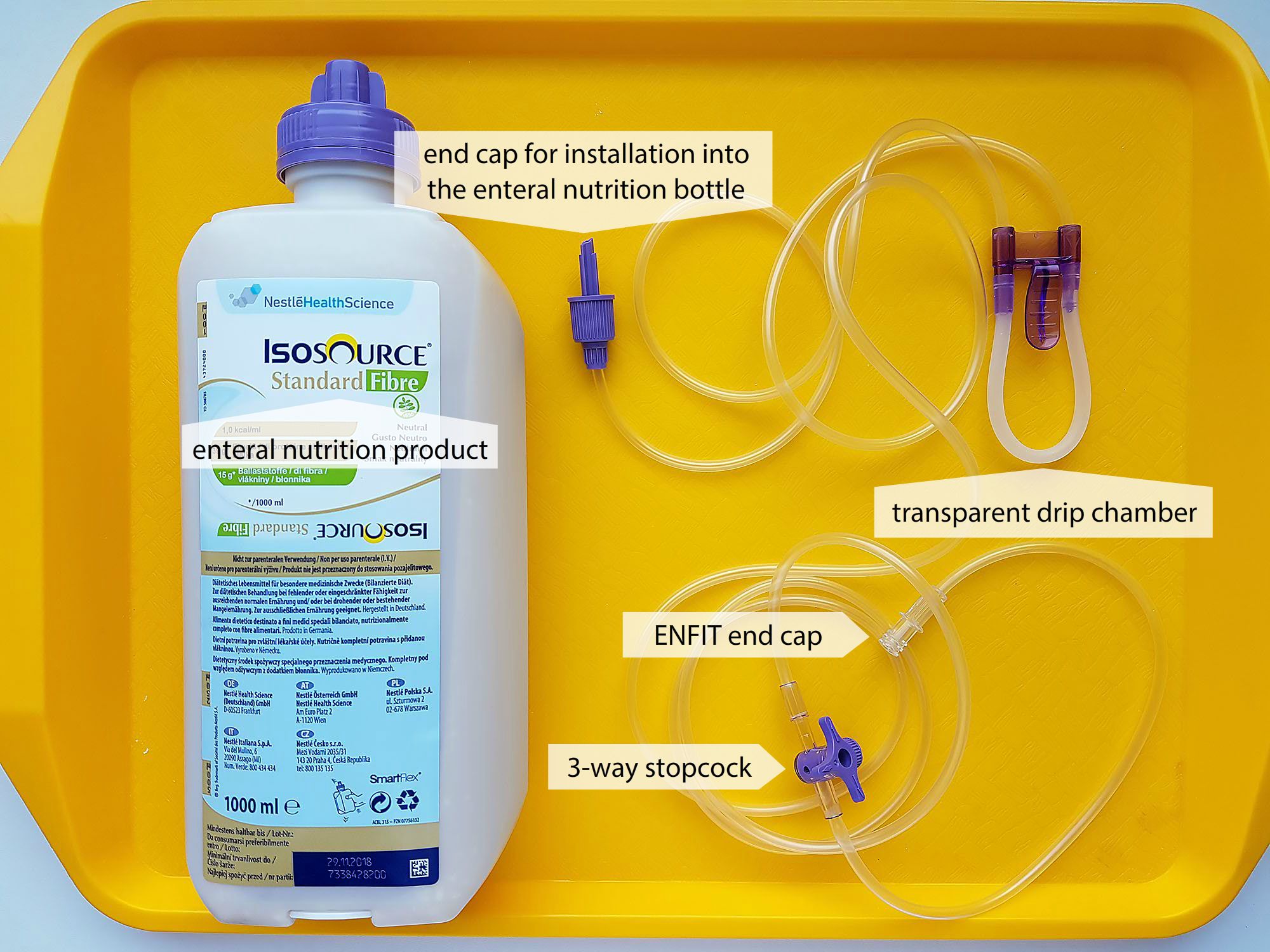
Continuous administration
- enteral pump (60–140 mL/hour)
- less risky (no risk of aspiration)
- overnight break




Nasojejunal tube (NJT)
- nutrition to the jejunum under sterile conditions (reduced risk of regurgitation, vomiting, aspiration)
- pharmaceutical nutritive products, nutritionally and chemically defined (Fresubin, Nutrison, Isosource)
- feeding by a pump for enteral nutrition
- continuous 24-hour administration, or with an overnight break
- tube is flushed regularly with half-normal saline solution or sterile water (at least 20 mL three times a day, always when feeding is interrupted and always when it is started again)
- feeding may be provided for several months, even at home (by patient or relatives)
- inserted by a doctor with nurse assistance
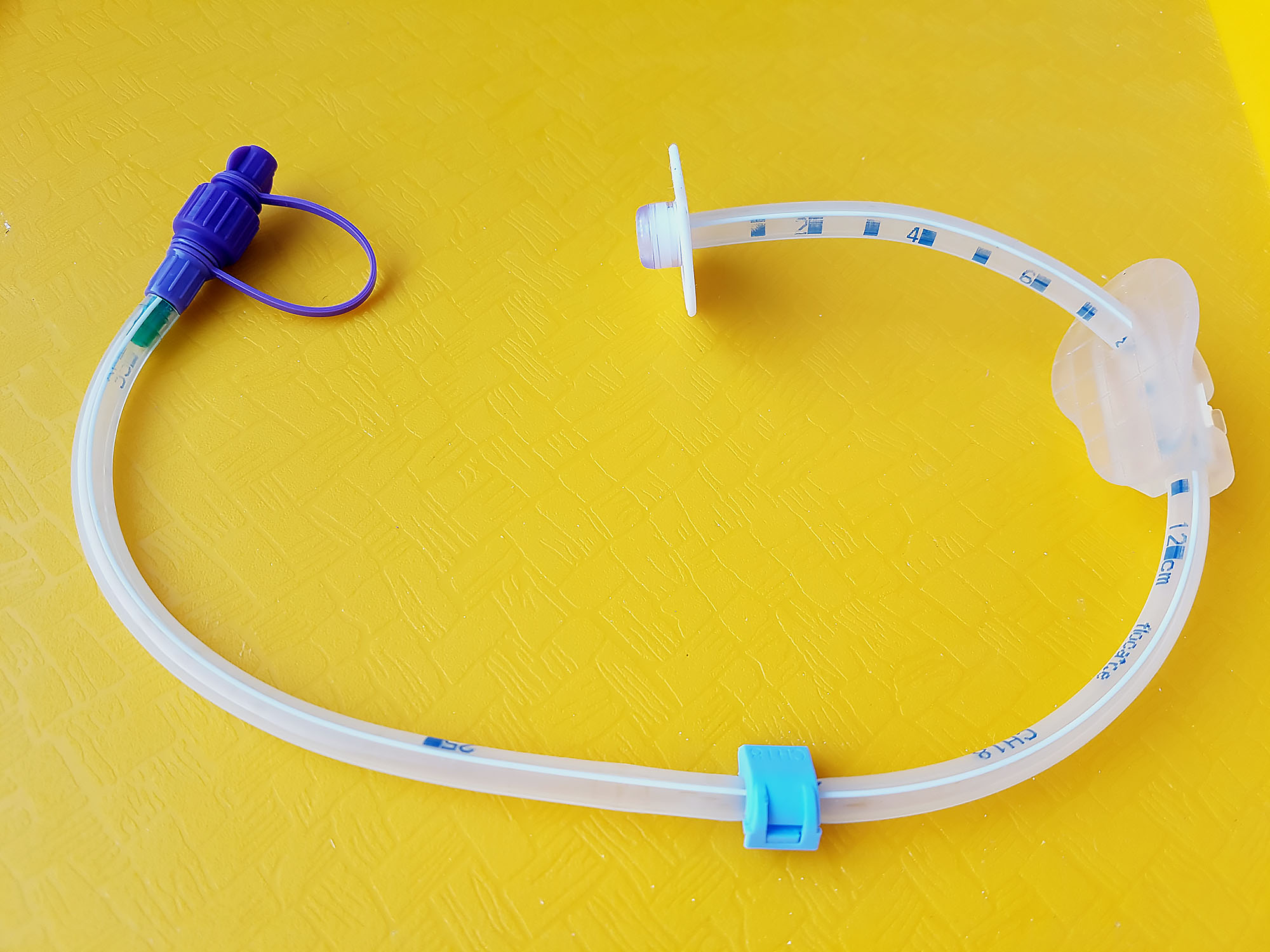
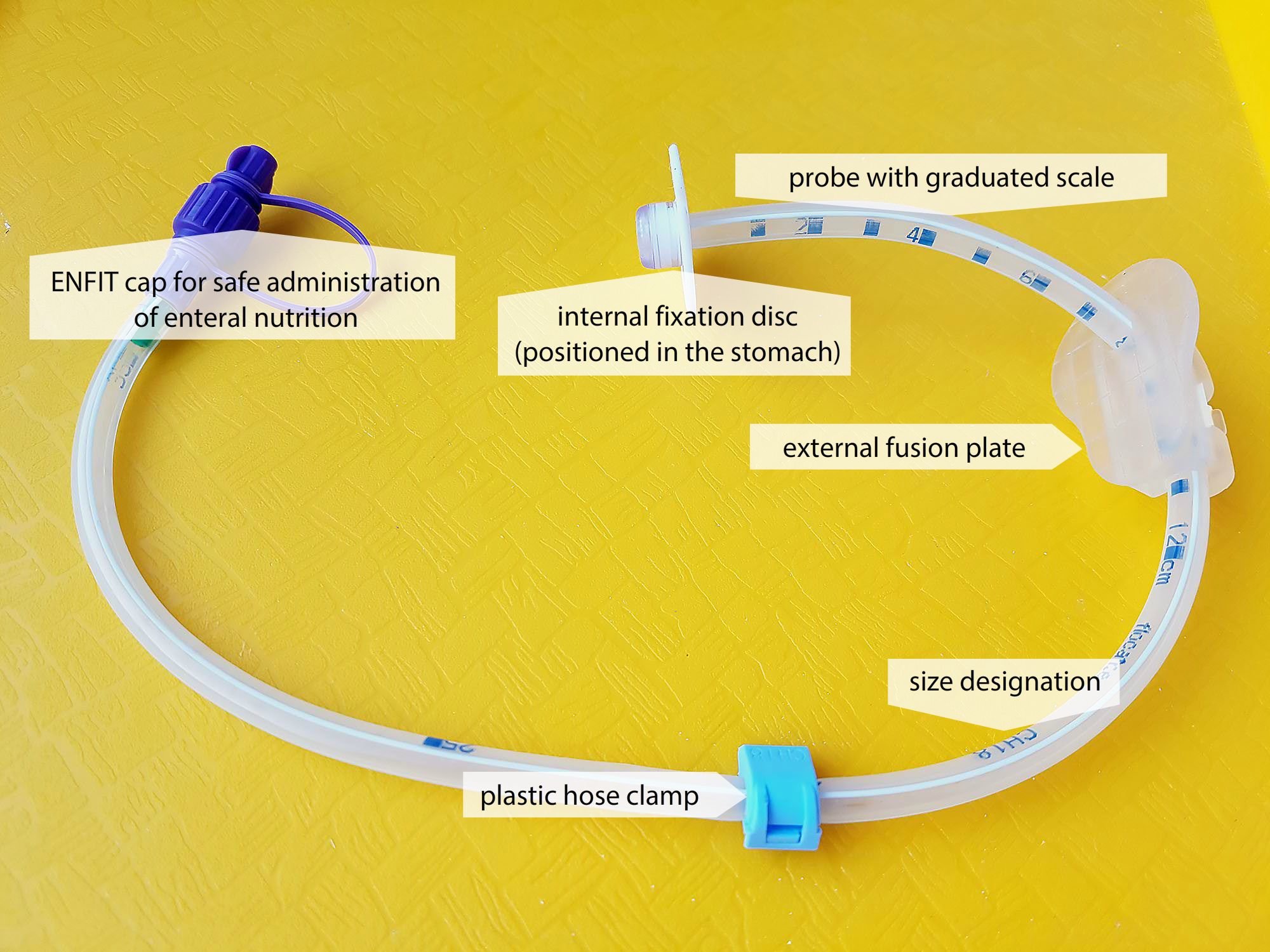
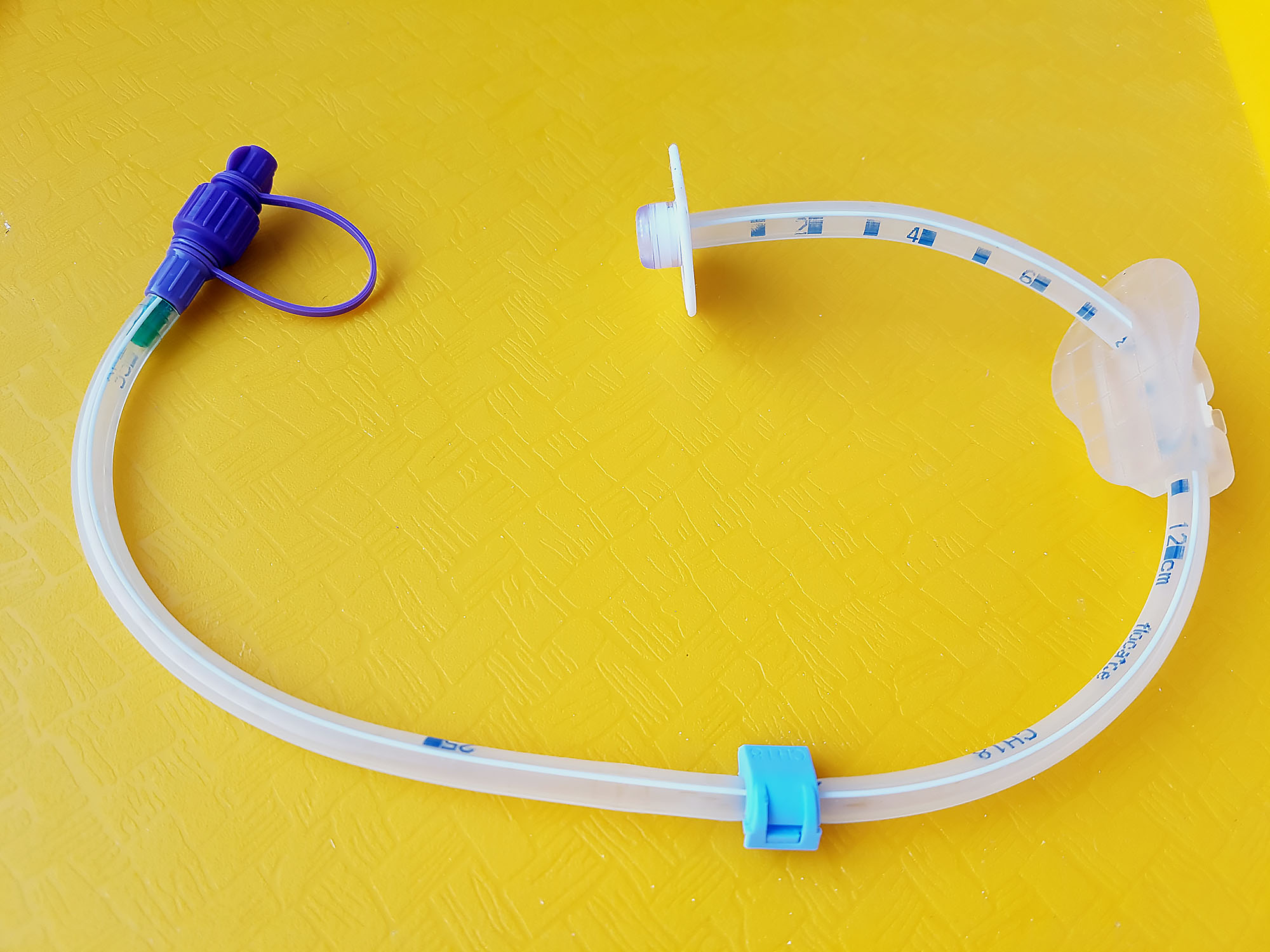
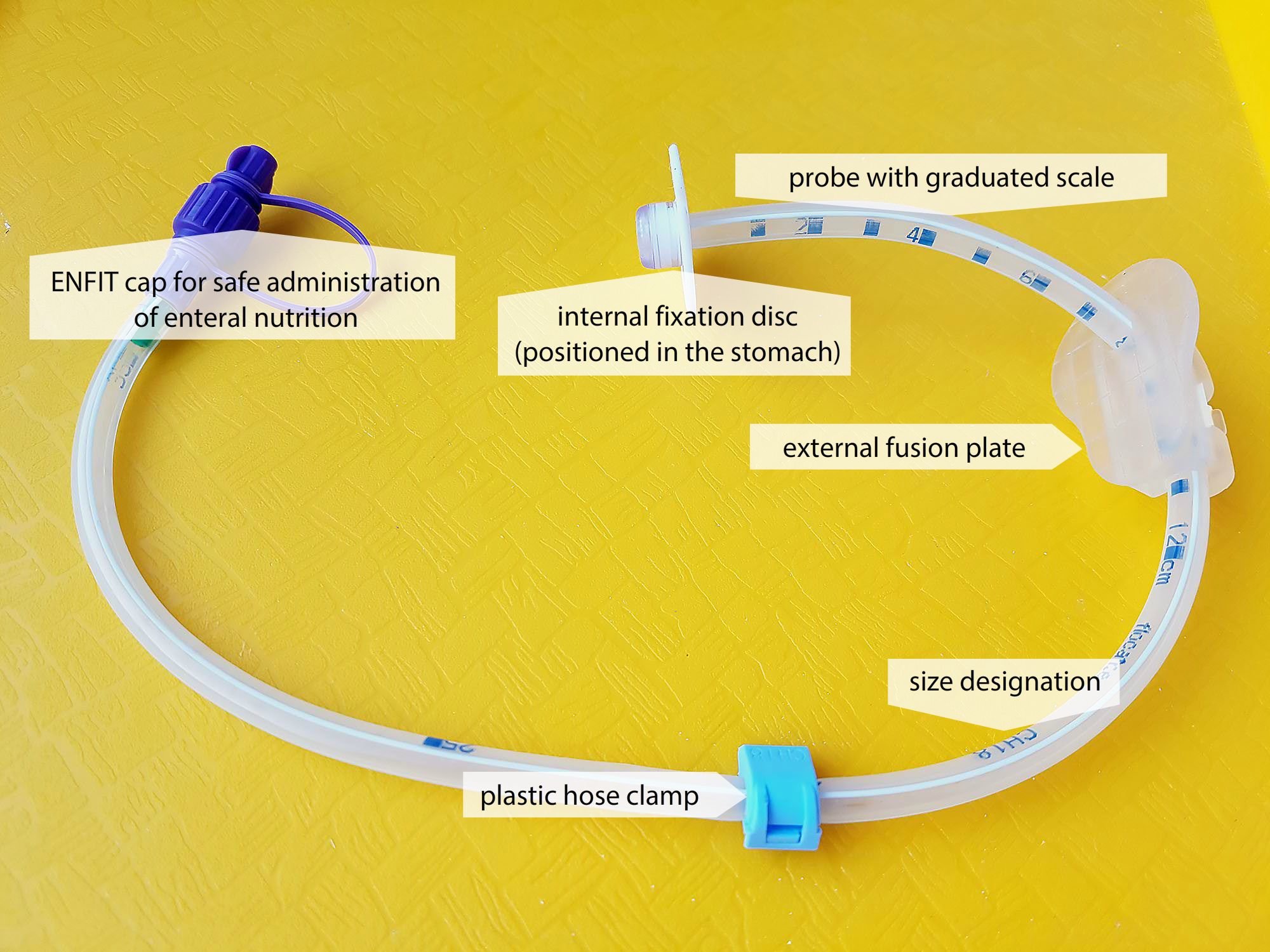
Percutaneous endoscopic gastrostomy (PEG)
- insertion of tube into the stomach through the abdominal wall with use of endoscope
- for long-term enteral nutrition (over 6 weeks)
- feeding bolus or continuously (as with NGT)
- rebandaging of the wound, tube rotation
- feeding for several months can be provided at home (by patient or relatives)












Percutaneous endoscopic jejunostomy (PEJ)
- Insertion of the tube into the jejunum through the abdominal wall using an endoscope.
- nutrition into the jejunum under sterile conditions
- for long-term enteral nutrition (over 6 weeks)
- pharmaceutical nutritional products, nutritionally and chemically defined (Fresubin, Nutrison, Isosource)
- feeding by a pump for enteral nutrition
- continuous 24-hour administration, or with an overnight break
- the tube is flushed regularly with sterile half-normal saline or sterile water
- rebandaging of the wound
- feeding for several months, can be provided at home (by patient or relatives)
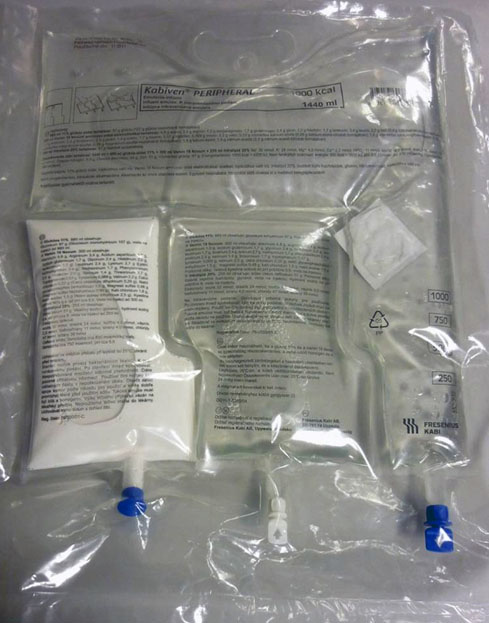
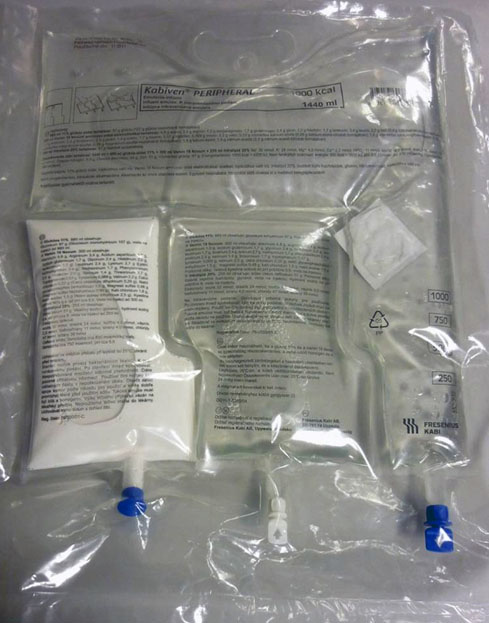
Parenteral nutrition
- method of delivering nutrients out of the digestive tract into the vascular system (directly into the bloodstream) – peripheral venous catheter, central venous catheter, venous port
- used for patients with dysfunctional digestive tract
- can be combined with enteral nutrition
- not a physiological route of nutrient administration
Purpose
- Ensuring the satisfactory nutritional state of the patient and the satisfactory state of his/her internal environment.
Methods of administration
To a peripheral vein
- short-term nutritional support
- risk of phlebitis
- solutions for hydration treatment (water, electrolytes)
- additional energetic intake – 5% Glucose
- supplementation of proteins and vitamins
To a central vein
- long-term nutritional support
- concentrated solutions without risk of phlebitis
- application to the subclavian vein
- application to the jugularis vein (end of the catheter in the superior vena cava)
- application to a venous port
Systems of administration
- multiple bottle system – single nutritional components in bottles (an obsolete system)
- all in one system – all nutritional components in one bag, the most frequently used
All-in-one bag
- bags prepared by manufacturer – the contents of the chambers are mixed just prior to the application
- bags prepared in the pharmacy according to the individual needs of the patient
- cyclically administered with an overnight break
Disadvantages of parenteral nutrition
- permanent venous access (risk of infection)
- unnatural way of eating (bypasses the digestive tract)
- risk of overdose
- impairment of the intestinal mucosa (atrophy, decrease in local immunity
- high price
Literature
- Jirkovský D. a kol. Ošetřovatelské postupy a intervence: učebnice pro bakalářské a magisterské studium, Praha, Czechia: Motol University Hospital, 2012. s. 389-411. ISBN: 978-80-87347-13-3
- Krišková, A. a kol. Ošetrovateľské techniky – metodika sesterských činností. Martin, Slovakia: Osveta, 2006. pp. 179-220. ISBN 80-8063-202-2
- Zeleníková, R. a Mandysová, P. Kontrola umístění nazogastrické sondy před zahájením enterální výživy u dospělých pacientů. Profese [online]. 2008, č. 2. http://profeseonline.upol.cz/archive/2008/2/POL_CZ_2008-2-6_Zelenikova.pdf Accessed May 11, 2016