In this chapter, the individual diseases are sorted according to their appearance in a way facilitating their differential diagnosis. The subchapters focus on the change of colour and surface of the oral cavity in the following manner: pigmented lesions, white/red lesions, erosions/blisters/bullae and ulcers. The character of those lesions is varied, with individual diseases differing in their etiology, pathophysiology and seriousness. The benefit of this sorting lies however in facilitating the differential diagnosis and the decision making – among other things because some lesions are very close to each other in appearance and cannot be reliably distinguished without a detailed examination.
In the areas of the lips and the tongue, we can also encounter similar manifestations of diseases with completely different etiopathogenesis; for this reason, the following sub-chapters include differential diagnostic remarks and schematic diagrams/overviews.
Pigmentations are less common on the oral mucosa than on the skin and usually found only incidentally. They are usually not associated with any subjective complaints, they can however represent an aesthetic problem if present in a visible area. Usually, they are represented by accumulation of a coloured substance in the epithelium or the tissue; some changes of vascular origin can however also have the appearance of pigmentations. The pigmented lesions can be of various colour and appearance and can differ in their severity, seriousness, prognosis and therapeutic approach. In establishing diagnosis, it is necessary to distinguish between physiological pigmentations (see Chapter 3.4) from the pathological ones (Chapters 5.2.4 a 6.3). On the one hand, these can represent completely benign conditions (physiological racial pigmentations, metallic pigmentations, smoker’s melanosis) but on the other, they can indicate serious diseases (lentigo maligna, malignant melanoma) or oral manifestations of some systemic diseases (Peutz-Jeghers syndrome, Addison’s disease).
This term encompasses a group of diseases, the most characteristic clinical symptom of which are white areas on the oral mucosa. The origin of these lesions varies – it can be caused by colonies of microorganisms (most commonly yeasts), by thickened epithelium with excessive keratinization or by a congenital disease.
The character of these lesions also varies. Using a single term to describe so many individual diseases differing both in etiology and pathophysiology can be however justified by the need to describe the differences among them necessary for diagnostic purposes and by the facts that their clinical appearance is almost identical and that they are very difficult to distinguish without a detailed examination. This group of diseases with white lesions includes in particular keratoses, stomatitis caused by cheek biting, leukoplakia, oral candidosis, oral lichen planus and mucosal changes of the lichenoid type. Less common diseases belonging into this group include white sponge nevus (nevus spongiosus albus), lupus erythematosus and psoriasis (Fig. 12).
A skin graft can also appear as a whitish-yellow discoloration of the mucosa in the lower alveolar region (it used to be transplanted at the lower alveolar process to improve conditions for retention of removable dentures).

Dif. dg. of diseases with oral white lesions as a prominent clinical symptom (Škach et al., 1975)
The basic form of the above mentioned diseases, i.e., of leukoplakia, oral lichen planus and oral candidosis, are white lesions (homogenous leukoplakia, reticular lichen planus, pseudomembranous candidosis). They can however manifest also as a red lesion (erythroplakia, erosive lichen planus, erythematous candidosis). Similar to the white lesions, diseases with red lesions are many and can differ both etiologically and pathophysiologically (Fig. 13).
The red lesions can represent:
atrophy – epithelial thinning. An example of this is atrophic glossitis, atrophic cheilitis, atrophic oral lichen planus, atrophic form of the lupus erythematosus.
erosions – the surface layer of the epithelium is disrupted by an injury, rupture of a vesicle, or immune process-induced apoptosis of keratinocytes.
inflammatory changes – these are characterized by an erythema caused by multiplication of capillaries in the submucosa. Examples may include drug-induced stomatitis, contact allergic reactions, erythematous candidoses.
submucous haemorrhage – manifests as petechiae, purpura, ecchymoses or a hematomas. They occur as a consequence of ordinary cheek biting or as a manifestation of haemorrhagic diathesis (thrombocytopenia/thrombocytopathy, vasculopathy, coagulopathy).

Dif. dg. of diseases with red lesions as a prominent clinical symptom
In these diseases, one must realize that a vesicle or a bulla on the oral mucosa is very susceptible to rupture and that the primary structure is therefore only rarely observed. During examination, we therefore usually either find erosions that can be tiny at the beginning and begin to combine and merge at a later stage (herpes and enterovirus infections) or extensive erosions covered by fibrin pseudomembranes (note: these do not represent a white lesion!) that are often formed due to a rupture of a bulla or epithelial necrosis (toxic-allergic reactions, drug-induced stomatitis, erythema multiforme, the bullous form of the oral lichen planus, pemphigus, pemphigoid). Erosions can however represent the primary structure formed by the disease (traumatic erosions). In particular, a timely identification of autoimmune blistering diseases is of utmost importance as early initiation of therapy significantly improves patients’ prognosis.
Diseases with erosions dominating the clinical picture can be in general categorized into several groups:
viral diseases – mostly caused by viruses of the herpes group
recurrent aphthous ulcers
toxic-allergic exanthemas
so-called blistering diseases – pemphigus, pemphigoid, Duhring’s disease (dermatitis herpetiformis Duhring), epidermolysis bullosa
In differential diagnosis, the clinician has to consider the clinical findings and structures associated with the findings – vesicles, erosions or bullae (Fig. 14-16). The algorithm for differential diagnosis of blistering diseases is shown in Fig. 17.

Differential diagnosis of erosions (amended from Škach et al., 1975)
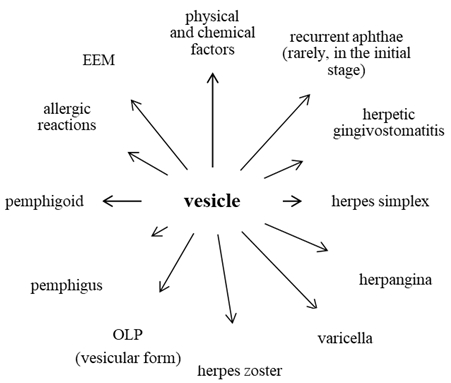
Dif. dg. of vesicular diseases (Škach et al., 1975)

Dif. dg. of diseases with a bulla as a principal structure (Škach et al., 1975)
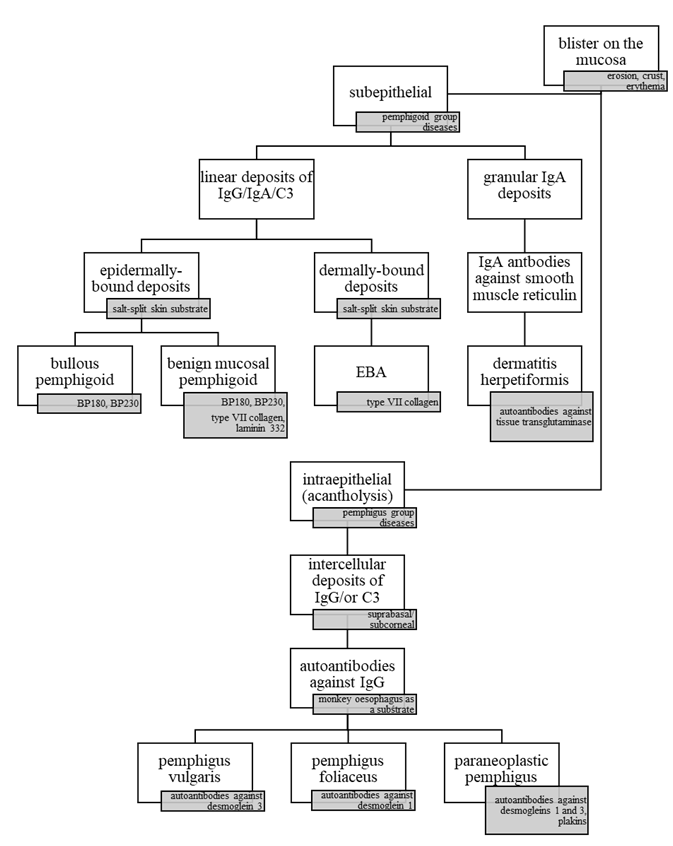
Dif. dg. of diseases with blisters as the principal structure (amended from Otten et al., 2014). The clinical finding must be augmented by a histopathological examination and subsequent direct and indirect immunofluorescence. Molecular-biological techniques such as ELISA, immunoblotting, immunoprecipitation, etc. often play a key role in the differential diagnosis.
Ulcers in the oral cavity can develop either as primary ulcers (traumatic ulcer, syphilitic ulcer, ulcers from burns/corrosion), or due to rupture of a blister (herpes zoster facialis) or bulla (pemphigus). The ulcers can vary in depth, deeper ones heal by scar. The difference between an erosion and an ulcer lies in the depth of the defect, clinical differentiation is however often impossible.
The following ulcerations are considered serious: carcinomas and other exulcerated tumours, haemoblastoses and agranulocytoses, deep invasive mycoses, syphilitic and tubercular ulcers.
Diseases that are dominated by ulcers as the main symptom in the clinical picture can be in principle classified (Fig. 18) into three main categories that will be discussed in the following subchapters.

Differential diagnosis of ulcerations (Škach et al., 1975)
The first group encompasses diseases with predilection to gingiva while remaining parts of the oral mucosa are only rarely affected. This group includes in particular necrotizing ulcerative gingivitis and mucosal changes in agranulocytosis and leukaemia.
The second group is on the other hand characterized by the fact that the ulcers primarily affect other parts of the oral cavity (any but the gingiva).
Traumatic ulcer is usually an acute, painful solitary lesion that heals well (after removing the etiological factor and a suitable local therapy).
Recurrent major aphthae are painful round or ovoid erosions or ulcers, one to two cm in diameter. They can occur as solitary lesions or in a group of two to three lesions. Healing lasts several weeks. It is always necessary to enquire about the presence of minor aphthae in the past.
Autoaggressive diseases from the pemphigus and pemphigoid groups manifest typically rather by extensive erosions covered with fibrin pseudomembranes than by typical ulcers. They last longer and sometimes can occur together with cutaneous manifestations or precede them. If pemphigus or pemphigoid are suspected, biopsy and laboratory examination (including direct and indirect immunofluorescence!) are necessary.
Ulcers developing due to burns/corrosive substances can be easily diagnosed based on questions while taking the patientʼs history. According to the exact cause of the defect (temperature or concentration of the corrosive substance and duration of exposure), either acute painful erosions or ulcers can develop. If corrosive substances are involved, it is always necessary to verify whether the patient swallowed the substance because of the risk of burns deeper in the GIT.
Acute haemoblastoses and bone marrow failure are accompanied with a major change of the patient’s general condition (exhaustion!) and systemic lymphadenopathy. The duration of the mucosal lesions is usually short (several days); haemorrhagic manifestations, gingival hyperplasia and painful mucosal ulcerations are observed. Suspected presence of these diseases requires immediate haematological examination.
Ulcers in systemic mycoses affect in particular the hard palate and the alveolar process of the upper jaw in immunodeficient persons. The disease progresses very rapidly.
Carcinoma of the oral mucosa – painless ulcer-like lesions may manifest months before the diagnosis. Pain usually only comes once nervous structures are affected. The ulceration usually shows palpable resistance, the ulcer is often irregular with rolled edges. In some patients, regional lymph nodes can be enlarged. If carcinoma is suspected, a histopathological examination is necessary.
Syphilitic chancre (1st stage) is a painless ulcer with elevated edges and hard floor surrounded by a notable collateral oedema – so-called initial sclerosis.
Tubercular ulcer in active lung tuberculosis is a solitary, deep and painful ulcer with rolled edges (tuberculoma) accompanied by enlargement of regional lymph nodes.
The third group consists of ulcers arising during specific inflammations – in our region, it is in particular tuberculosis and syphilis. From the perspective of dentistry, such specific inflammations count among the diseases endangering the personnel and representing risk of professionally acquired infection. The knowledge of the disease and adherence to the hygienic principles are crucial as is the knowledge in the field of diagnosis and occurrence of the oral form of such diseases.
If evaluating the inflammatory changes of the lips, it is necessary to consider the specifics of lips when compared to the other parts of the oral mucosa. The disease can affect the skin of the lip, the vermilion zone and/or the mucosal part. Sometimes, all three parts of the lips can be affected, sometimes only one of them; lesions on each of them however have their specifics. The fact that individual infection agents can have predilection for a certain part of the lips must be taken into account. For example, impetigo can be only found on the cutaneous part as well as folliculitis or furuncles (for which the presence of the skin adnexa are a necessary prerequisite) while recurrent aphthae can only affect the mucosal part of the lips.
Příčiny | Objektivní nález | ||
|---|---|---|---|
Physical |
mechanical |
erythema, excoriation – cheilitis simplex, cheilitis exfoliativa, fissures, erosions, ulcers, crusts |
|
thermal |
erythema, vesicles, eschar |
||
radiation |
phototoxicity |
cheilitis actinica (solaris, abrasiva) |
|
photoallergy |
cheilitis venenata |
||
radioactivity |
erythema, ulcer |
||
Chemical |
burns (acids, bases) |
eschar (bases – grey; acids – depends on the acid; e.g. after nitric acid – yellowish; after sulphuric acid – dark to black; after hydrochloric acid – white) |
|
|
pigments |
cheilitis exfoliativa (desquamation of the upper epithelial layers) |
||
Infections |
viral |
herpes labialis |
|
bacterial |
ulcer, gangrene |
||
cocci |
furuncles, phlegmon, impetigo, erysipelas, painful corners of the mouth |
||
TBC |
swollen lips, ulcer |
||
syphilis |
primary – erosion, ulcer secondary - erosion, plaques muqueuses + opalines, condylomata lata tertiary – gumma (rare) |
||
fungal |
painful corners of the mouth (with other factors)) angular candidosis |
||
Allergies |
plant antigens, animal antigens, food proteins, chemicals |
eczema, Quincke’s oedema |
|
Other diseases |
EEM – blisters, erosions, crusts pemphigus – blisters, erosions, crusts OLP, LE – erosions, crusts, lichenoid changes cheilitis granulomatosa in Melkersson-Rosenthal syndrome – lip oedemas |
||
in salivary gland heterotropia |
cheilitis glandularis simplex (cheilitis of Puente) cheilitis glandularis aposthematosa (of Volkmann) cheilitis glandularis suppurativa (Baelz)) |
||
Painful lesions of the corners of the mouth can be caused by various factors. The predisposing conditions differ with age. Often, such lesions are caused by a mixed fungal-bacterial infection. The infection usually develops in macroscopically undetectable cutaneous and mucosal defects in the areas that are susceptible to infection by these conditionally pathogenic organisms (anguli infectiosi). Other causes may include lack of some vitamins (vitamins B2, B6, B12, folic acid) and/or minerals (Fe).
The region of the corners of the mouth is predisposed towards salivary maceration, licking and drying, which results from its anatomical structure. The corner of the mouth can be divided into three zones:
cutaneous zone (skin, outer) covered by normal skin including all adnexa.
transition zone (vermilion) covered by a squamous cell epithelium of the vermilion with smaller degree of keratinization. Of the skin adnexa, sweat and sebaceous glands are missing as well as the apocrine and hair follicles.
mucosal zone (inner) covered by non-keratinizing epithelium of the oral mucosa with orifices of tiny salivary glands.
Clinical picture: If the course disease is atypical, the corners of the mouth (cutaneous or transition zones) contain markedly erythematous painful patches with a central fissure. Sometimes, a whitish border can be found in the neighbourhood of such patches. The lesion is usually bilateral and its course depends on many factors. In children, painful corners of the mouth can occur in rare congenital cutaneous fistulas that can be susceptible to secondary infection. There are many other predisposing factors in children – various (bad) habits such as biting the oral mucosa and/or lips, licking the vermilion zone, putting various objects in the mouth and chewing them, etc. Microtraumatic lesions of the corners of the mouth get easily infected, which can lead to secondary infection, most commonly streptococcal impetigization) and thus to the further trauma of the tissue.
In adults, the painful corners of the mouth also occur relatively commonly as the number of local and systemic predisposing factors grows. The skin partially loses its elasticity, submucous connective and adipose tissue, the bite height is reduced due to abrasion of the hard dental tissue or loss of supporting zones. The most important systemic factors include diabetes mellitus, Sjögren syndrome, malignant tumours and many other diseases.
Etiopathogenesis remains unknown; aside of congenital predisposition, other etiologies are considered such as functional disorder of the autonomous nervous system, inflammatory or allergic reactions to various microbial agents, or an immunity-mediated reaction to various components of the diet. The histopathological findings include a granulomatous inflammation, lymphostasis and accumulation of the lymphocytes in the tissue. Younger individuals (regardless of their sex) are more susceptible to this disease. A typical triad of symptoms is detailed below; some of them can however be missing in a particular patient at the same time:
granulomatous cheilitis - recurrent lip oedemas occur in 80 % of patients. An asymmetrical oedema of one or both lips turns into macrocheilia over the course of several days as a result of the granulomatous inflammation. Sometimes, it can spread into the surrounding tissues – cheeks, eyelids, face including the forehead, ears and neck. In the oral cavity, it can affect the buccal mucosa, tongue, the mucosa of the hard palate, sometimes hypertrophic gingivitis.
paresis of the facial nerve - usually peripheral, a central paresis with a unilateral tinnitus, vertigo and migraine-like headache can be however also present..
lingua plicata (potentially accompanied by macroglossia)
Rarely, organ symptoms can manifest, such as dysphagia, aphonia, attacks of asthma, megacolon, etc. Complete ad integrum recovery is rare.
Th.: Causal, corticoid depot injection can be applied, in some cases surgical therapy.
Dif. dg.: In particular, we must rule out other causes of swelling in the lips: odontogenic inflammation, cheilitis glandularis, angioedema, sarcoidosis, Crohn's disease, lymphangioma or the tumor process.
We speak about macroglossia/microglossia if the tongue is larger/smaller than normal. Of course, significant individual deviations from the normal size are possible – a reliable diagnosis can be only established if the deviation is major and causes problems. Reasons of macro/microglossia vary, we can classify them as congenital and acquired.
Congenital macroglossia results from thickening of the muscle tissue (macroglossia muscularis), or can represent a diffuse lymphangioma or hemangioma (macroglossia lymphangiomatosa et hemangiomatosa). A partial macroglossia can be caused by struma lingualis or cysta ductus thyreoglossus. Macroglossia can also be a part of many other diseases, such as Down syndrome or cretinism (congenital hypothyreosis) due to a massive deposition of mucopolysaccharides in the muscle tissue of the tongue, the tongue can protrude from the mouth.
Congenital microglossia can also be a part of rare congenital craniofacial and extracranial anomalies. Hypoplasia of the tongue is usually associated with developmental disorder in the period between the 4th and 6th week of intrauterine development.
Acquired macroglossia can be a consequence of haematopoiesis disorders (amyloidosis), metabolic disorders (glycogenoses), diseases of endocrine glands (myxoedema, acromegaly) or syphilis (syphilitic gumma).
Tumours causing enlargement of the tongue are not too common. Usually, they represent vascular anomalies such as lymphangioma (capillary, cavernous, cystic or, if multiple tumours are present, lymphangiomatosis) or haemangioma. Unlike lymphangioma, bluish discoloration can be seen through the mucosal surface in the latter as it is filled with erythrocytes (important for differential diagnosis). Focal enlargement of a part of the tongue can be caused by neurofibroma (Schwann cells tumour) – at that site, it is especially in association with Recklinghausen disease (neurofibromatosis).
Pseudobulbar palsy can cause microglossia due to a spastic cramp. If one-sided, the tip of the tongue aims to the affected side.
The base coating of the tongue is formed by the epithelial parts of the filiform papillae that project above the level of the mucosa. Other parts of the coating (peeled-off epithelium, cellular detritus, saliva, bacterial microflora and food remnants) are its minor components. The intensity of the coating is determined by numerous processes, the foremost of which is the condition of the filiform papillae – their density, length and degree of keratinization. Other factors include the temperature and consistence of the food, chewing motor process and intensity (or reduction thereof in paralysis, loss of consciousness, etc.).
Physiologically, a thin whitish coating is normally present on the tongue. Such coating can be found in healthy individuals, its intensity however even in such people varies throughout the day both ways, depending on the daytime and food. The coating is usually the most intensive in the morning as the epithelial cells that peeled overnight and microorganisms are on the surface. In certain pathological conditions, however, the coating is either thickened or pathologically reduced.
The coating of the tongue is diagnostically very important. The tongue changes its appearance in various stages of a disease and it cannot be said that the manifestations are specific for some diseases (e.g. the so-called “strawberry tongue” in scarlet fever can also occur in other exanthema associated diseases such as measles). The condition of the coating is rather a general indicator of the condition of the organism at any given moment. A dry, thickly coated, brownish tongue is a sign of a generally bad condition of the organism (typical e.g. for septic states). If the disease progresses, the coating sometimes creates a “skin-like” coating. When the patient’s condition improves, such “second skin” usually separates and a coating-free smooth tongue appears. Filiform papillae develop again within 2-4 weeks, which is, together with the moisturizing of the mucosa, a sign of recovery. A coating-free (smooth) tongue also indicates a metabolic disorder or circulatory insufficiency. As mentioned above, both extremes can develop over the course of a single disease.
The increased thickness of the coating arises as a result of induration and increase in length of the filiform papillae and of increased keratinization of its epithelial projections. Acute coating develops rapidly, often within 24 hours of the onset of the disease. It is usually associated with serious acute diseases – serious infections (pneumonia, meningitis, sepsis, scarlet fever) or shock-associated diseases (acute abdomen, coma, serious myocardial infarction). In these diseases, the tongue self cleaning is affected, the organism is dehydrated and high fever occurs. The tongue is often dry, with very obvious thick brown coating – individual papillae appear as if glued together (forming a kind of film) – fuligo linguae.
Besides this type, there are also other forms of acutely increased coating. As an example, we can mention a “fresh”, whitish coating that can be found in herpetic gingivostomatitis or allergic conditions. The tongue in this type of coating is moist (unlike in fuligo).
Pathologically increased tongue coating in chronic conditions is mostly associated with chronic lesions of the GIT. Such coating is often termed dyspeptic coating. It however may be present only during a certain stage of the disease, namely during exacerbation (of dyspepsia, gastric ulcer, gastritis, etc.). It does not reach the intensity of the acute coating, is often less obvious. A specific type of chronically increased coating of the tongue is lingua villosa nigra.
There are many transition states – from almost normal coating, through a coating in which filiform papillae are missing their keratinized prominences, up to a complete atrophy of the papillae. The coating may be lacking either across the entire tongue, or only on its parts. Most commonly, this is visible in nutritional deficiency syndromes such as in vitamin B-complex or Fe deficiency, in nutritional deficiency in cachectic states (hepatic cirrhosis, malignant diseases), or in Sjögren syndrome. The reduced coating of the tongue or its complete disappearance can also result from some drug intoxications (e.g. after Au or barbiturates intoxication).
Pathological changes of the tongue in deficiency states are usually termed by the traditional term glossitis, although strictly speaking, this term should from the pathological perspective only describe an inflammatory disease of the tongue. A more accurate term would probably be a “glossopathy” (or deficiency-associated lingual coating disorders). This group of diseases is etiologically variable.
The appearance of the deficiency-associated tongue is mostly atrophic, smooth (sometimes even glossy – completely without papillae). Mostly, it is atonic, smaller in size, with reduced tissue turgor, fissures or ulcerations may be sometimes present. The colour depends on etiology – pale red in anaemic diseases, dark red in hepatic cirrhosis, livid in cachexia. The patients complain about pain, burning or itching of the tongue. Deficiency-associated glossitis can appear in many diseases with negative metabolic balance – in inflammatory or malignant diseases, afflictions of GIT, malabsorption, disorders of hepatic functions (including alcoholism), uraemia, chronic cardiac insufficiency and many other pathological conditions.
The surface of the tongue can be divided according to the composition of the mucosa divided into two types. While the changes on the bottom of the tongue usually represent only a part of diffused changes of the lining mucous membranes, the mucosa of the dorsum of the tongue is usually the only affected surface and the clinical picture of the inflammation results from the structure of the dorsum of the tongue. Many changes on the tongue can be associated with multiple systemic diseases (glossitis atrophica can result from anaemia, avitaminoses or toxic effects of various substances). It is also necessary to assess the dynamics of the changes („wandering“ changes in lingua geographica). In the inflammations of the lingual mucosa, superficial (exudative) inflammations that only affect the mucosa must be distinguished from deep (interstitial) inflammations that penetrate deep into the mucosa.
Causes | Objective findings | ||
|---|---|---|---|
| Developmental deviations on the dorsum of the tongue | lingua plicata, lingua geographica | ||
Physical |
mechanical |
erythema, fissures, erosions, necrosis, ulcer (traumatic glossitis) |
|
thermal |
erythema, vesicles (erosions), necrosis, ulcer |
||
electrogalvanic |
erythema, erosion, ulcer, lichenoid and hyperplastic changes |
||
Chemical |
burns (acids, bases) |
eschar (bases – grey; acids – colour varies according to the particular acid) |
|
pigments, antiseptics |
lingua villosa nigra |
||
others (smoking) |
leukoplakia, lingua villosa nigra |
||
Infections |
viral |
glossitis in herpetic gingivostomatitis, herpes zoster |
|
bacterial |
abscess, phlegmon, noma (if the organism is weak) |
||
cocci; streptococci |
strawberry tongue (scarlet fever) |
||
staphylococci |
glossitis profunda, abscesses of the tongue |
||
TBC |
primary - ulcer secondary - tuberculoma |
||
syphilis |
primary – erosions, ulcer secondary – erosions, plaques muqueuses + opalines, lisses tertiary – gumma, glossitis interstitialis luetica, lingua lobata |
||
fungal |
oral candidosis, glossitis rhombica mediana, lingua villosa nigra; systemic mycoses |
||
Allergies |
plant antigens, animal antigens, dietary proteins, chemicals, haptens |
Quincke’s oedema, glossitis venenata |
|
Immunopathological diseases |
recurrent aphthae – ulcer, erosions (only major aphthae can manifest on the dorsum of the tongue) OLP – white lesion EEM – erosions covered by a fibrin pseudomembrane pemphigus, pemphigoid |
||