The thorough knowledge of both macroscopic and microscopic structure of tissues at physiological conditions is necessary for being able to assess pathological changes of the oral mucosa. Fig. 1 shows the structure of individual segments of the oral mucosa compared mutually and with the skin.
The principal features distinguishing the mucosa from skin include:
colour – the mucosa is pink in the areas with the keratinized epithelium (which is caused both by the thinner layer of the stratum corneum and by a higher degree of blood supply) while the red colour is more intense in the areas with incomplete cornification.
moisture – caused by the saliva secretion.
absence of skin appendages
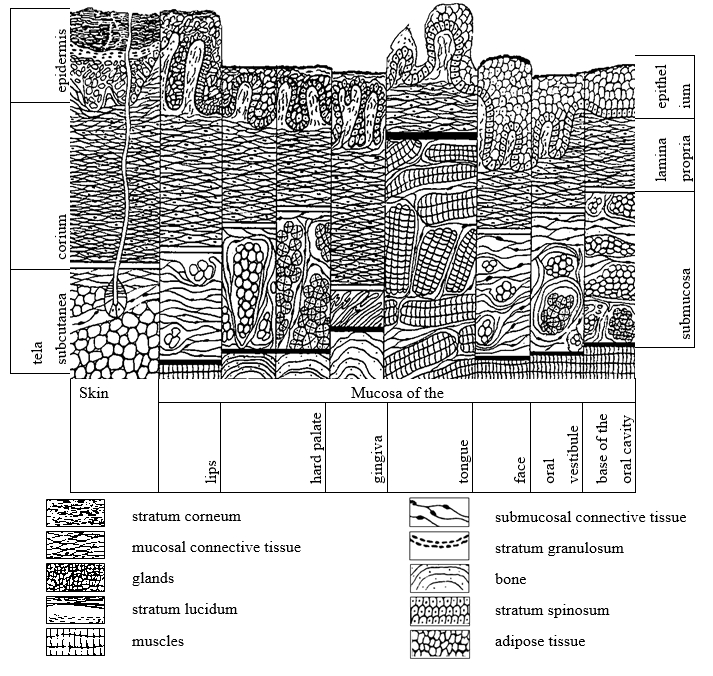
A schematic view of the microscopic structure of the skin and oral mucosa (Škach et al., 1982)
From a topography point of view, the oral mucosa can be divided into several regions that correspond with the anatomy of jaws and attached muscles. The following types of the mucosa are recognized: buccal mucosa, labial mucosa, alveolar mucosa, palatine mucosa including the uvula and frontal palatine arches, the mucosa of the oral base and the tongue. The oral mucosa consists of stratified squamous-cell epithelium, the properties of which vary according to the function, i.e. to the load to which it is exposed (they differ in the presence or absence of the cornified layer on the surface of the mucous epithelium):
Sliznice ústní dutiny je tvořena epitelem vrstevnatým dlaždicobuněčným, jehož vlastnosti se liší podle funkce, tzn. podle toho, jaké zátěži je vystaven (rozdíl je v přítomnosti či absenci keratinizující vrstvy na povrchu slizničního epitelu):
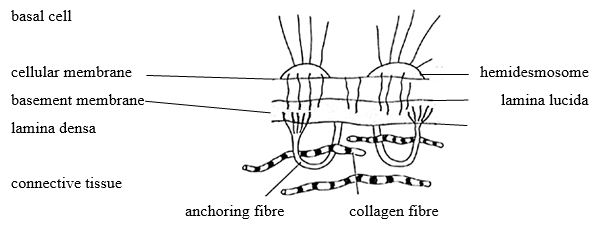
The ortho-keratinizing epithelium can be found on the hard palate, alveolar mucosa and attached gingiva; it has four layers – stratum basale, stratum spinosum, stratum granulosum and stratum corneum. Layers resemble the epidermis of the skin but are substantially thinner and the stratum lucidum is absent (Fig. 2).
The para-keratinizing epithelium covers the remaining parts of the oral mucosa (i.e., vestibular mucosa, buccal mucosa, soft palatine mucosa, sublingual region). It has two layers - stratum basale and stratum spinosum.
A specific position between the skin and the mucosa is attributed to the vermilion zone (also called lip red). Clinically, it resembles the oral mucosa while histologically, it resembles the epidermis with keratinization without the presence of most skin appendages (hair follicles, skin glands) and without the presence of salivary gland ducts.

Other types of cells are present among epithelial cells (keratinocytes) in the basal layers of the mucous epithelium, such as melanocytes (forming and accumulating the pigment melanin) or Langerhans and dendritic cells (antigen-presenting cells) that are involved in immune reactions. The epithelium on the dorsum of the tongue forms duplicatures, i.e. papillae that can take several forms: filiform papillae, fungiform papillae, circumvallate papillae, or foliate papillae. Filiform and fungiform papillae form the basis of the physiological coating of the tongue; foliate papillae are predominantly located along the side of the tongue whereas circumvallate papillae are located on the border between the body of the tongue and the root of the tongue, accommodating taste receptors.
The cells of the stratum basale are attached to the basement membrane (Fig. 3). This fibrous membrane is located between the epithelium and lamina propria mucosae. It is folded in various ways – depending on the height of the papillae of lamina propria and the depth of the rete ridges. The density of interdigitation (the interlocking of epithelial and fibrous parts) determines the mechanical resistance of the mucous membrane. The lamina propria mucosae consists of a thin collagen tissue penetrated with elastic fibres, cellular elements (fibroblasts, fibrocytes, histiocytes, heparinocytes), blood and lymphatic vessels and nerve endings, which gradually turns into the submucous fibrous tissue (except for the dorsum of the tongue where it is firmly attached to the lingual aponeurosis (aponeurosis linguae) or into the periostal ligament (the alveolar process, hard palate). The submucous tissue contains tiny (minor) salivary glands (serous, mucinous or mixed) practically in the entire oral mucosa; those glands permanently produce small amounts of saliva, thereby keeping the oral mucosa wet and lubricated.
Generally, the following three types of oral mucosa can be distinguished according to the function of individual segments:
Specialized mucosa: the dorsum of the tongue
"Functional” (masticatory) mucosa: palate, attached gingiva
"Non-functional” (lining) mucosa: remaining parts of the oral cavity