Specimen Collection – blood
- venous, capillary, arterial
- coagulated and non-coagulated blood
- venepuncture – frequently requested method of obtaining blood specimens from vein, “closed” systems are preferred (e.g. SARSTEDT, VACUTAINER, etc.)
- venous blood collection from central venous catheter (jugular vein, subclavian vein) – turn off all infusions and intravenous pumps, use strictly aseptic technique, use correct adapter, gently aspirate 10 mL of blood and then aspirate desired amount of blood, reclamp catheter
- skin puncture (capillary puncture) – the least traumatic method of obtaining a blood specimen – puncture a vascular area on the finger or earlobe or heel (little children), frequently requested methods: blood glucose monitoring, ABGs (arterial blood gases), blood count
- arterial puncture – radial artery, femoral artery
Principles
- prepare equipment + blood tubes
- inform the patient about purpose of the procedure
- respect security principles and standards – use disposable gloves, aseptic technique
- identify the patient using two identifiers (name, birthday – “What's your name?” “When were you born?”, check identity wristband
- commonly recommended orders: serology, biochemistry, coagulation, haematology, erythrocyte sedimentation















*taping the venepuncture site with sticking plaster after the blood collection is not generally recommended – moving and self-sufficient patients compress the venepuncture site with sterile tampon themselves
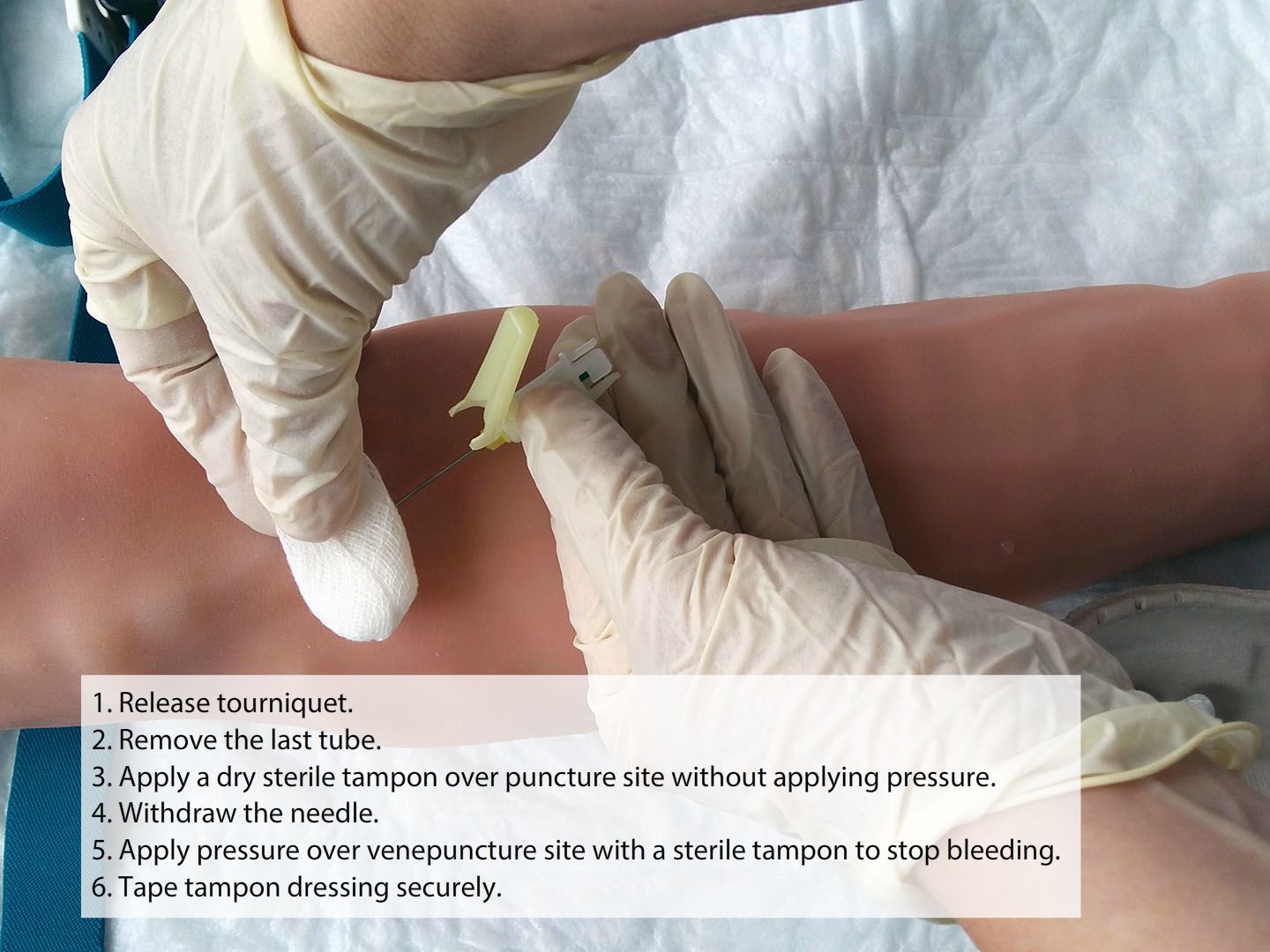
*taping the venepuncture site with sticking plaster after the blood collection is not generally recommended – moving and self-sufficient patients compress the venepuncture site with sterile tampon themselves

Venous blood collection
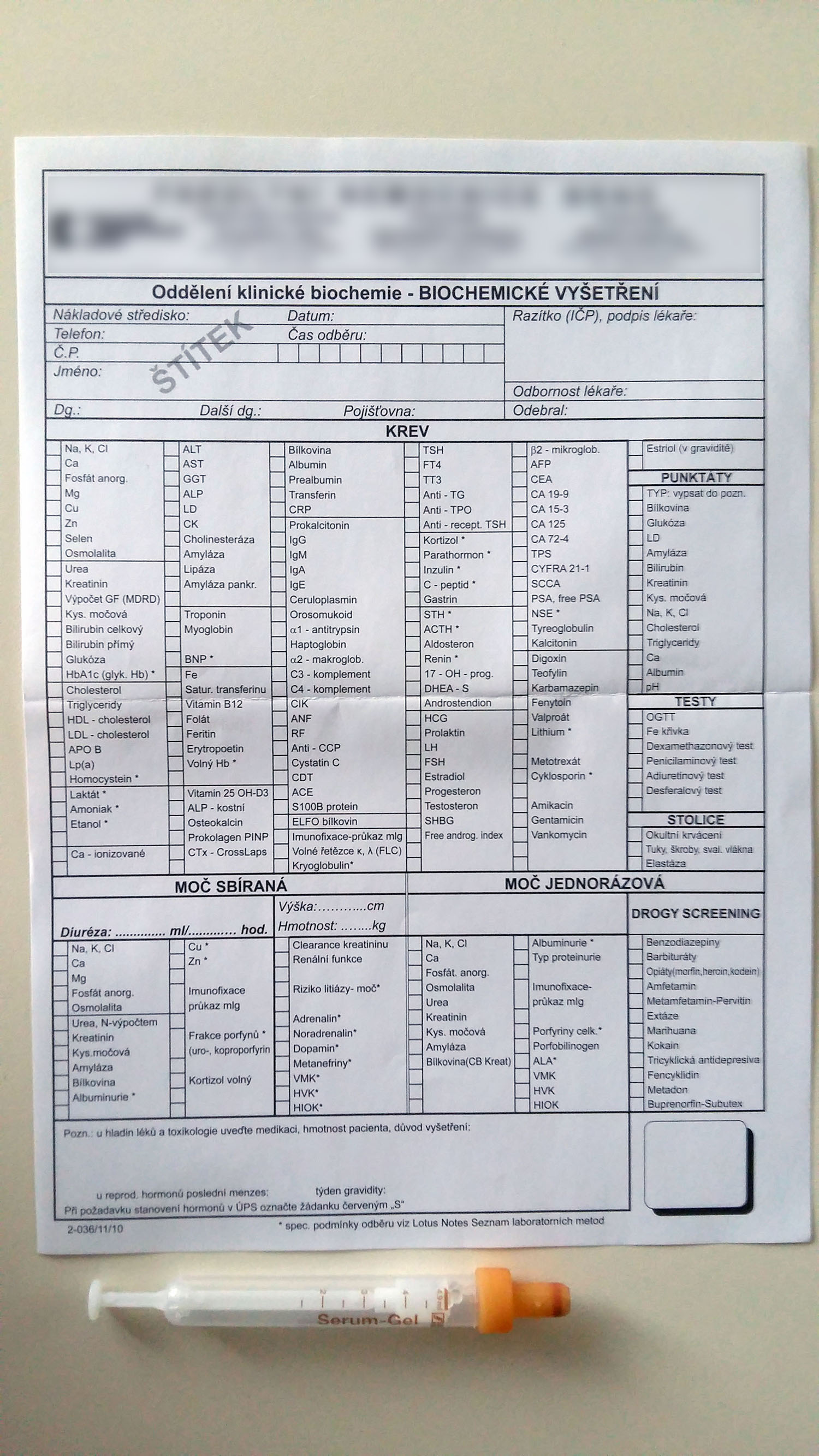
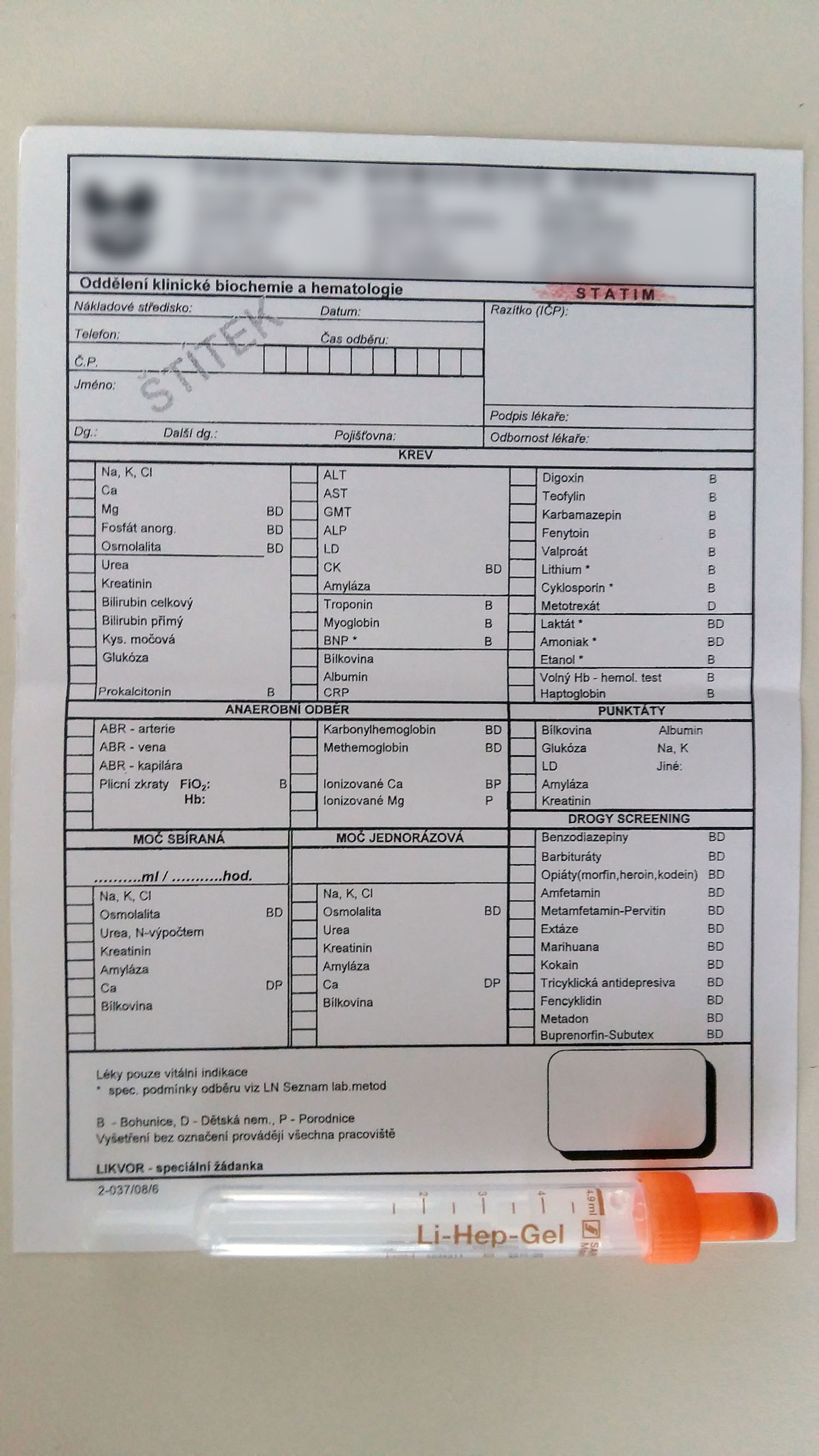
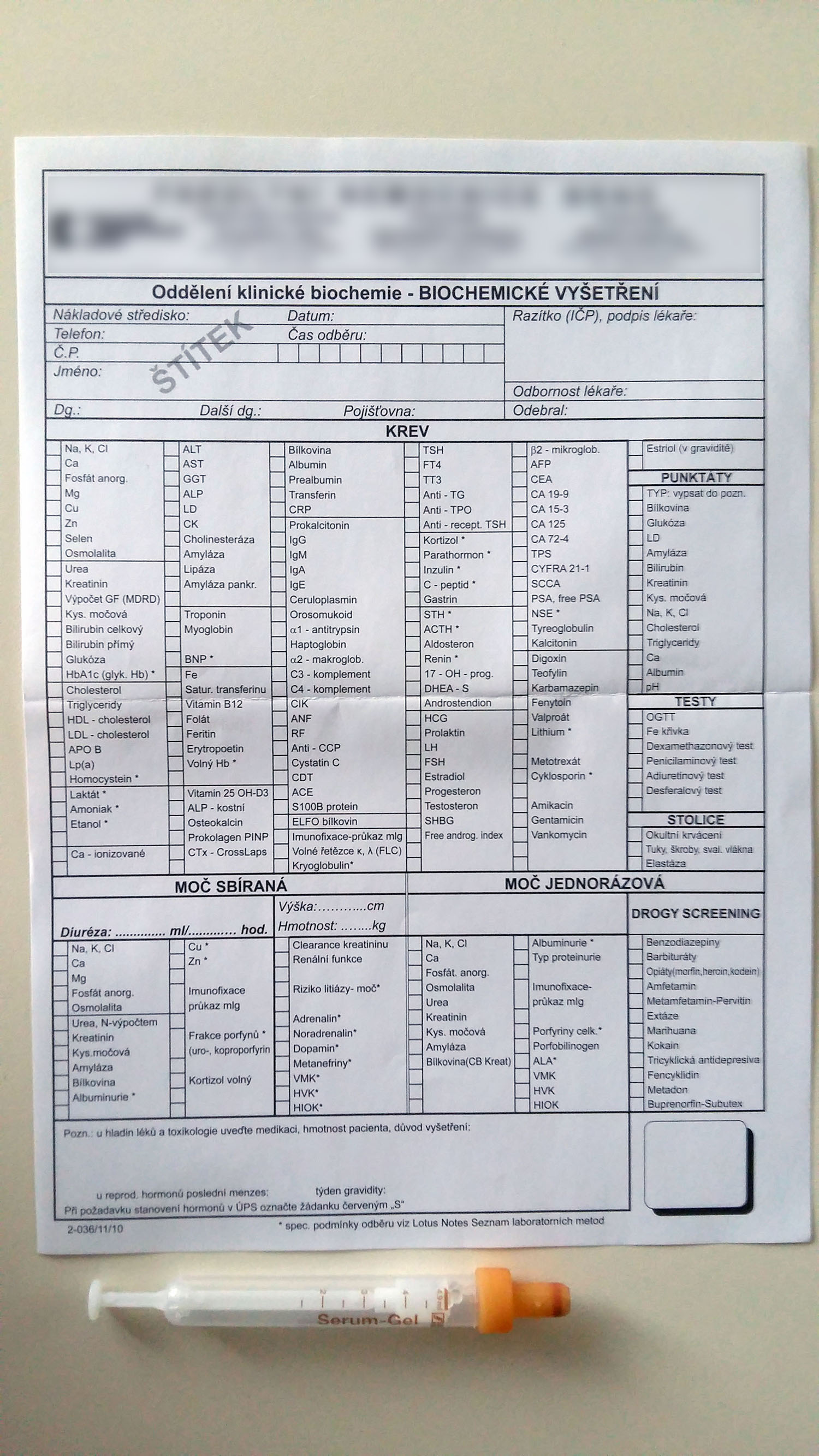
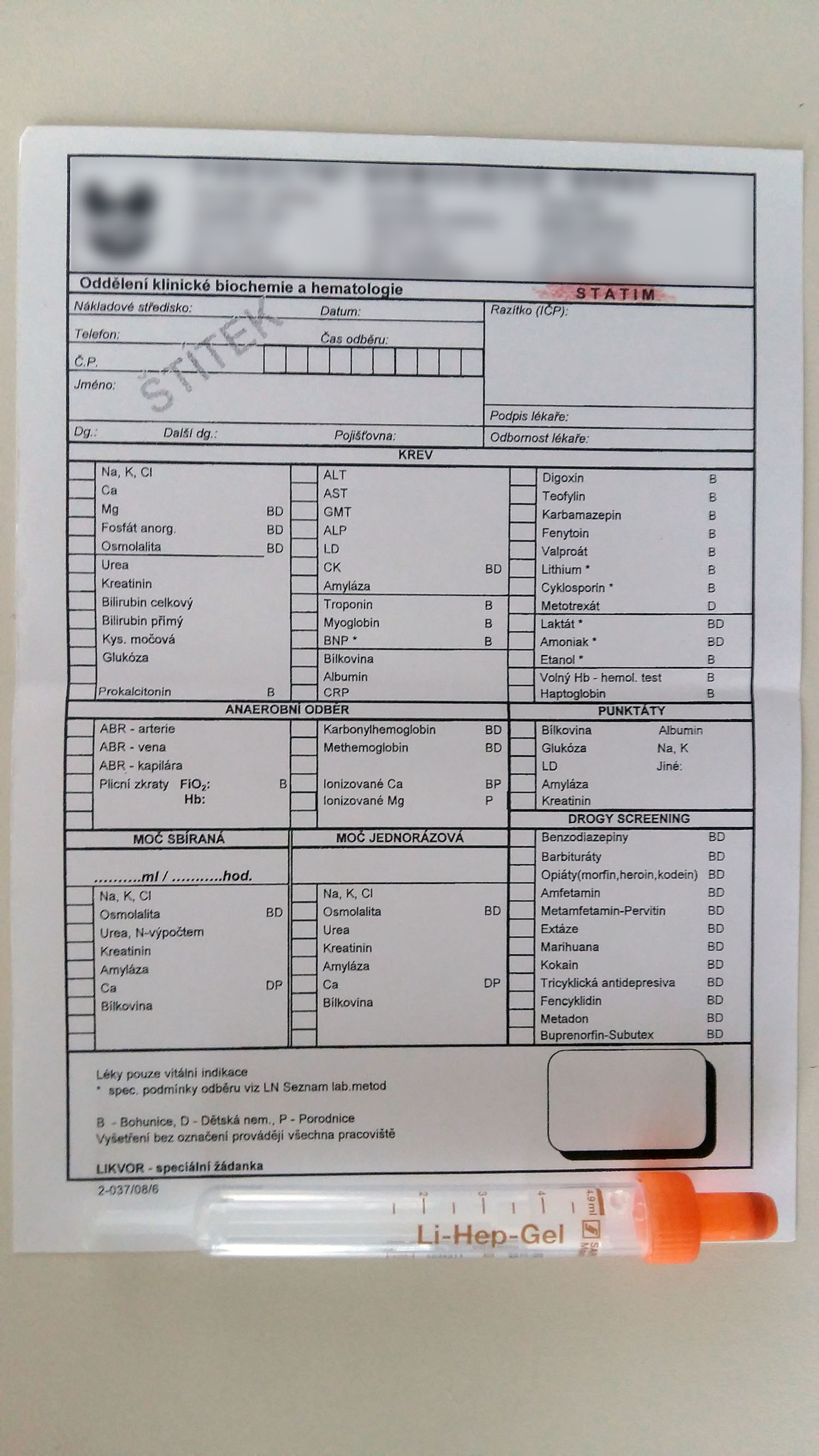
Biochemical examination of venous blood
- coagulable venous blood
- routine blood collection – standard analysis period, brown designation of the blood tube (Sarstedt monovette 4,9 mL)
- STATIM examination – results are available within 2 hours of specimen's admission to the laboratory, orange designation of the blood tube (Sarstedt monovette 4,9 mL)
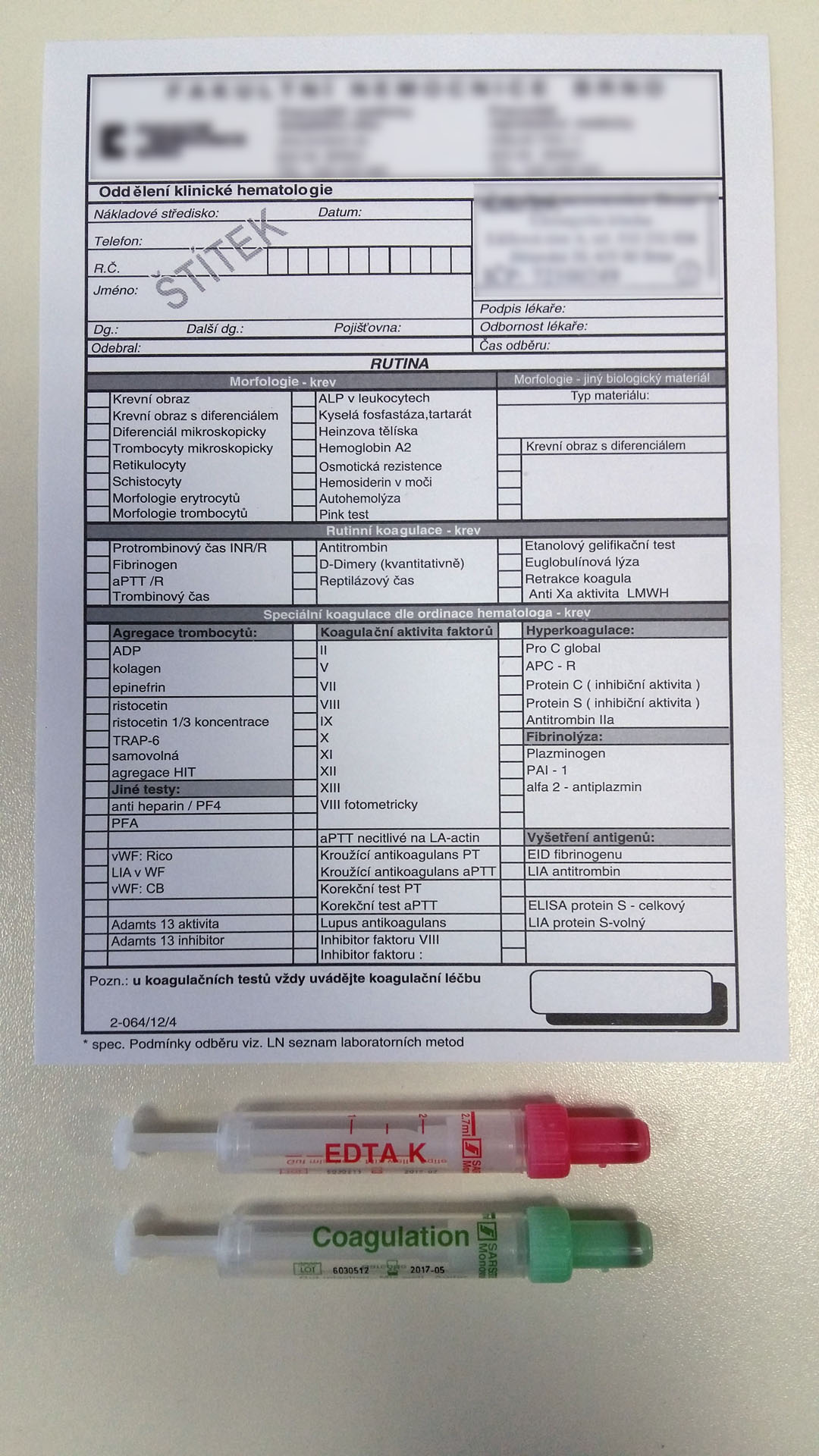
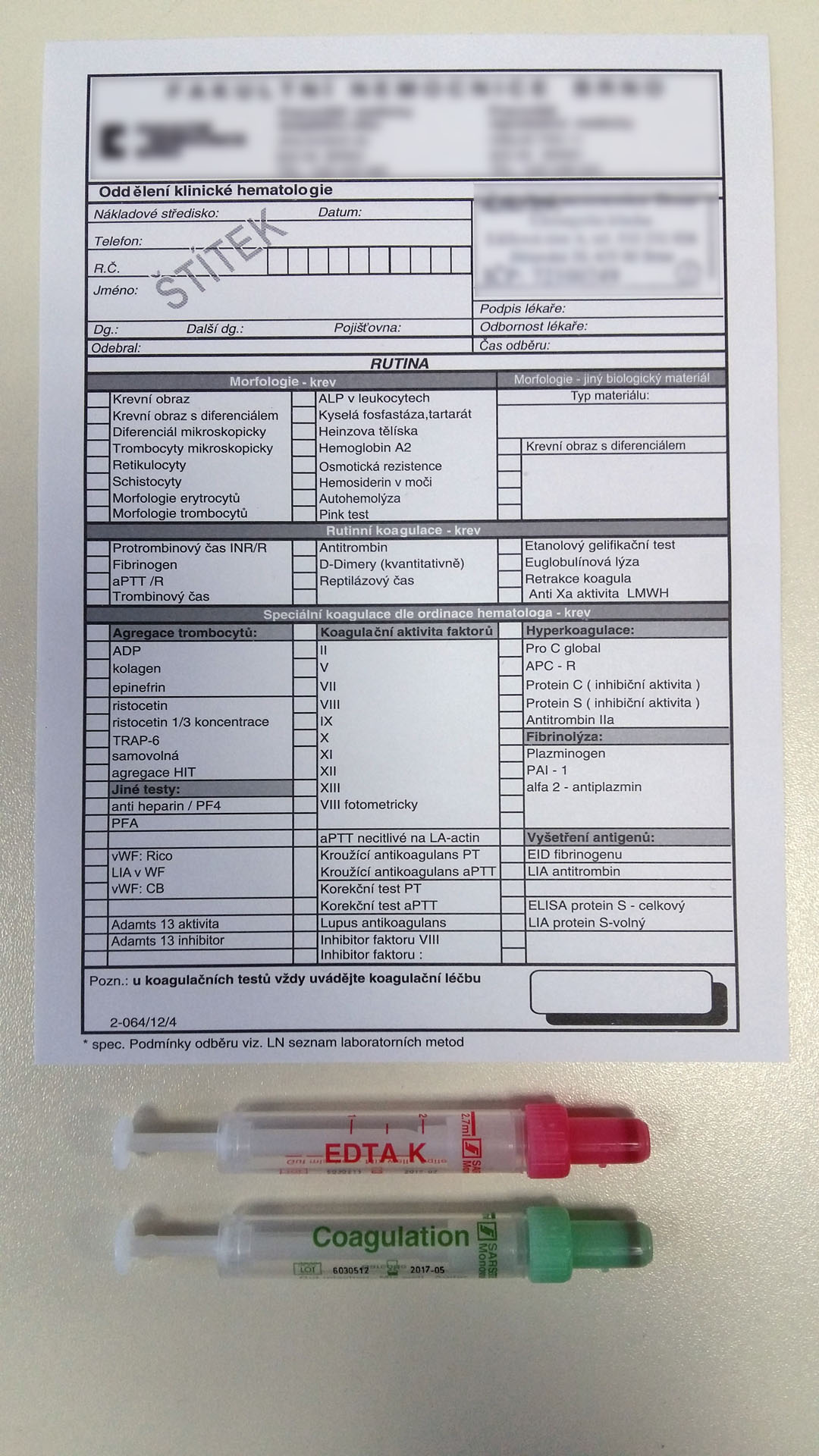
Haematologic examination of venous blood
- non-coagulable venous blood
- morphology – form and quantity of blood elements
- complete blood count – red designation of the blood tube (Sarstedt monovette 2,7 mL)
- frequently requested blood examinations: blood count (BC) – also known as a complete blood cell count (CBC); full blood count (FBC); or full blood exam (FBE) – in Czech use designation “KO” in patient medical chart (record form). BC gives information about blood cells: leukocytes, erythrocytes, thrombocytes, haemoglobin, haematocrit
- differential blood count – use designation KO + diff. in record form; examination of blood count and differentiation of leukocytes
- complete blood count – red designation of the blood tube (Sarstedt monovette 2,7 mL)
- haemoocoagulation – coagulation of blood (blood clotting)
- haemocoagulation examination – green designation of the blood tube (Sarstedt monovette 3 mL).
- indicate the dose and time of anticoagulant, antiplatelet, LMWH therapy in request form
- the most common coagulation tests are
- Prothrombin time test (PT – velocity of passage of extrinsic blood coagulation; result in INR (international normalized ratio) – in patients taking Warfarin
- APTT (activated partial thromboplastin time – velocity of passage of intrinsic coagulation pathway; result expressed in seconds
- Xa factor – monitoring of anticoagulation therapy Heparin, fibrinogen (factor I – blood protein produced in liver that is changed into fibrin to clot the blood when body tissue is damaged)


Blood bank
- non-coagulable venous blood
- blood group and Rh factor examination; ordering of transfusion products
- Sarstedt monovette 4,9 mL or 5 mL – red or green designation of blood tube (according to the practice of the workplace)


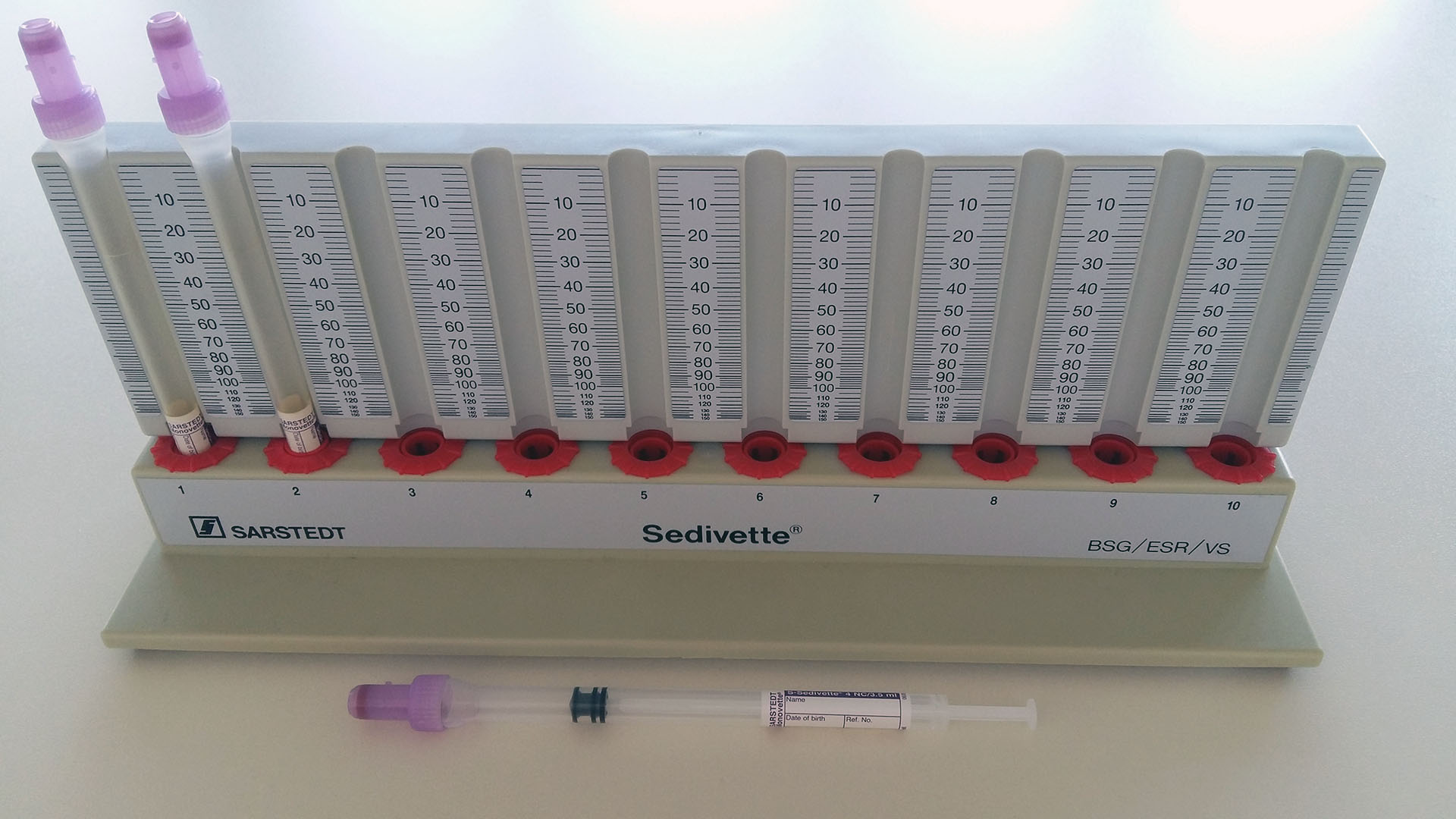
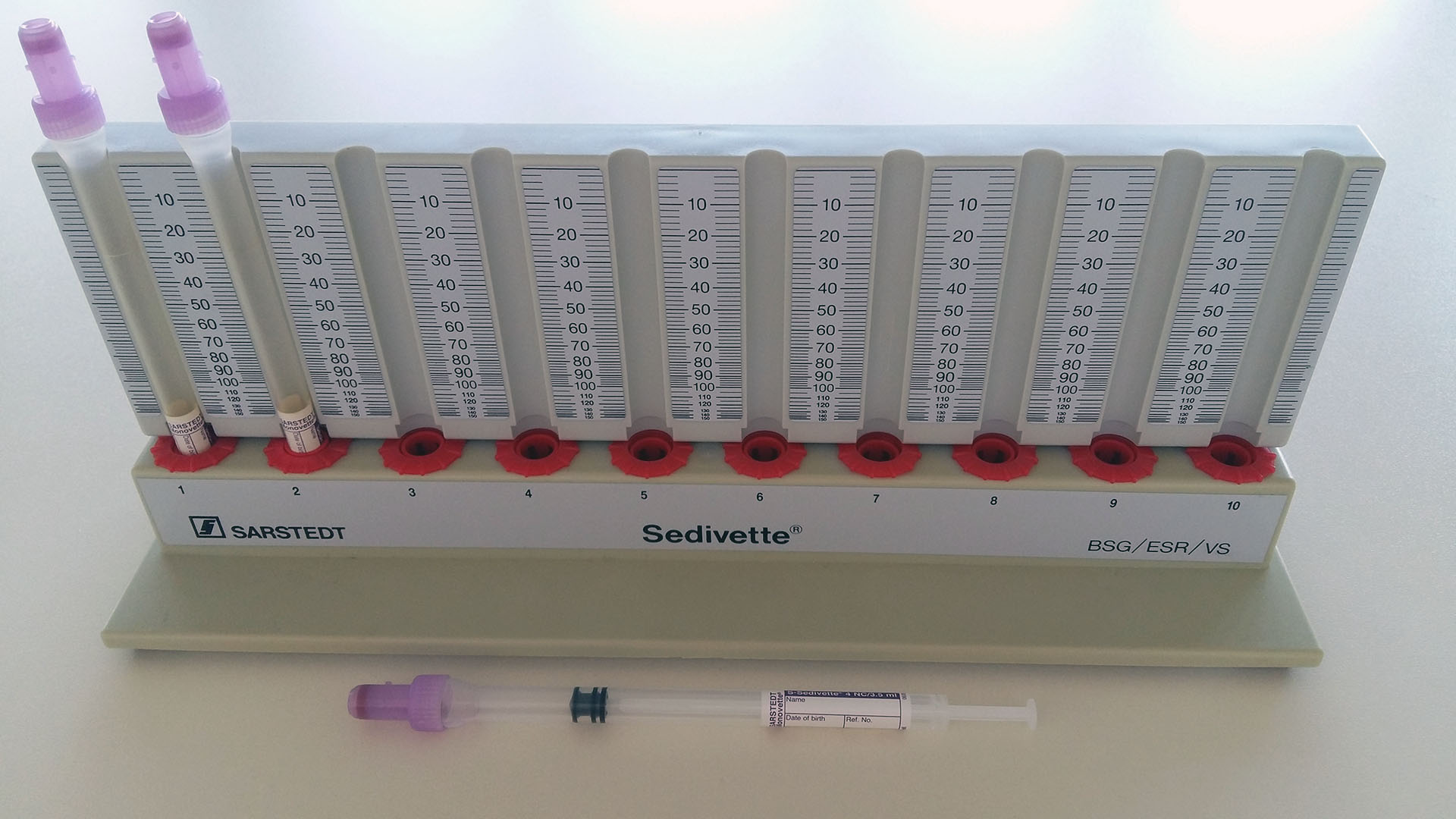
Erythrocyte sedimentation rate ESR (FW = Fåhraeus-Westergren)
- non-coagulable blood from vein
- Sarstedt monovette violet designation
- examination can be done at a department or outpatient office, or can be sent to a biochemical laboratory
- Subtract the value after one and two hours (female reference range 8/12, male reference range 5/8).


Serological examination
- coagulable venous blood
- Sarstedt monovette 4,5 mL (white designation)
- serum antibody level analysis
- examination
- BWR – Bordet-Wassermann test (antibody test for syphilis)
- WR – Widal test (for typhoid fever)
- PBR – Paul-Bunnel test (antibody test for mononucleosis)
- Rheumatoid factors: ASLO – anti-streptolysin 0 (streptococcal infections, autoimmune diseases); LATEX – latex fixation test (latex agglutination – tests antibodies for rheumatism)
- anti-HIV (tests antibodies for HIV)
- HBsAg – “Australian antigen” (surface antigen of the hepatitis B virus – tests for hepatitis B positivity)


Microbiological blood examination – blood culture (haemoculture)
- coagulable venous blood
- open blood collection system – blood collection into a 20 mL syringe, application of collected blood into aerobic and anaerobic haemocultivation vials with specific medium, or into a special vial for antibiotic therapy; exchange needle before application into the bottle, 1 vial = approx. 8–10 mL of blood
- blood is collected using aseptic technique, thorough disinfection of the injection site (according to the practice of the workplace); according to the doctor's orders, make skin swab after disinfection (negative result of the swab = proof of sufficient disinfection)
- prevention of contamination of the sample to prevent false positivity
- request form for bacteriological examination


Capillary blood collection
Blood glucose monitoring
- non-coagulable capillary blood
- blood glucose detection
- glycaemic reference values of 3.6–5.6 mmol/L (possible deviations according to glucometer or laboratory settings.)
- pre-meal collection – preprandial blood glucose; post-meal collection – postprandial blood glucose.
- Glycaemic profile
- Small glycaemic profile – 4x blood collection: 30 minutes before eating (breakfast, lunch, dinner) + at 10 p.m. (according to the practice of the workplace)
- Large glycaemic profile – 7–9x blood collection – 30 minutes before eating (breakfast, lunch, dinner) + one hour after meal + at 10 p.m. + at 2 a.m.+ 4 a.m. (according to the practice of the workplace)
Methods of taking blood glucose
- glucose meter – professionally recommended devices such as ACCU-CHEK (designed for POCT = Point Of Care Testing = bed side test); personal glucose meters are primarily designed for self-monitoring in patients with diabetes mellitus
- yellow Eppendorf tube = examination in biochemical laboratory
Principles of blood glucose collection
- puncture sites – lateral side of finger (index finger, middle finger, little finger), well vascularized area, warm, do not massage or press the puncture site, instead apply a “sliding press” on the entire finger from the palm towards the puncture site
- disinfect the puncture site
- use a lancet if possible; avoid using standard needles (cannot estimate penetration depth)
- wipe off the first drop, take the next drop to the test strip or to the sampling tube (haemolysis of the sample causes false value of the blood glucose)
- record glycaemia in the documentation; the ACCU-CHEK glucometer stores information automatically in electronic documentation










Examination of capillary blood gases (CBGs)
- non-coagulable arterial blood
- examination of oxygenation and ventilation by measuring arterial blood gases, examination of acid-base balance
- collection into a heparinized capillaries
- principles: sucking in blood without air bubbles, inserting the metal wire and capillary closure, moving the magnet over the outer wall of the capillary (mixing of the sample material with the anticoagulant).








Arterial blood collection
Arterial blood gas test (ABG)
- non-coagulable arterial blood
- most common sampling points – radial artery, femoral artery
- examination of arterial blood gases provides valuable information about patient's respiratory and metabolic disturbances
- In Czech, you will find ABR or Astrup designation in patient's record
- Arterial blood collection into a heparinized tube – Sarstedt monovette – white tube with orange designation 2 mL.
Principles
- physician performs the collection
- cover the collection site with sterile dressing and compress for 10–15 minutes
- if the sample is taken from femoral artery, ensure compression by using a sachet with sand
- if the sample is taken from radial artery, perform compression by palpation, or a TR Band radial compression aid may be used, after approx. 30 minutes check sterile coverage, check whether the puncture site is bleeding
- collection must be processed in the laboratory within 15 minutes





